The rapid expansion of telehealth services has revolutionized healthcare delivery, particularly since the COVID-19 pandemic catalyzed widespread adoption. While virtual care offers unprecedented access and convenience, healthcare organizations face significant hurdles in provider credentialing, a critical but often overlooked aspect of telehealth implementation. Below, the complex credentialing challenges in telehealth and practical solutions to streamline these processes.
The Telehealth Credentialing Conundrum
Telehealth credentialing sits at the intersection of regulatory compliance, patient safety, and operational efficiency.
Unlike traditional in-person care models, telehealth introduces unique complexities to the credentialing process:
Multi-State Licensing Requirements
For healthcare organizations with providers serving patients across multiple states, this means:
- Managing different application requirements
- Tracking varying renewal timelines
- Navigating state-specific scope of practice regulations
- Understanding telemedicine-specific rules that differ by jurisdiction
Credentialing Verification Organization (CVO) Limitations
Traditional CVOs weren’t designed with telehealth’s unique challenges in mind.
Their processes often lack:
- Integration with telehealth platforms
- Systems for tracking multi-state licenses
- Efficient methods for managing digital credentials
- Solutions for rapid privileging during public health emergencies
Payer Enrollment Complexities
For successful reimbursement, providers must be properly enrolled with numerous insurance payers across different states.
This creates several pain points:
- Each payer has unique enrollment requirements
- Enrollment timelines can stretch 90-180 days
- Requirements change frequently without standardized notification
- Telehealth-specific billing credentials may be required
Time and Resource Constraints
The administrative burden of telehealth credentialing is substantial. Many organizations report dedicating 1.7x more resources to credential telehealth providers compared to traditional providers. This strains already limited healthcare administration resources.
Strategic Solutions for Telehealth Credentialing Challenges
While the challenges are significant, innovative solutions are emerging to address telehealth credentialing pain points. These range from regulatory improvements to technological advances.
Embracing Interstate Compacts and Reciprocity
Interstate licensure compacts offer one of the most promising solutions for multi-state practice challenges.
The Interstate Medical Licensure Compact (IMLC)
The IMLC streamlines the licensing process for physicians practicing across state lines. Currently, 38 states, DC, and Guam participate in this compact.
For eligible physicians, the IMLC offers:
- An expedited pathway to multi-state licensure
- A streamlined application process
- Reduced administrative burden
Other Relevant Compacts
Similar compacts exist for other healthcare professionals:
- Nurse Licensure Compact (NLC)
- Physical Therapy Compact (PT Compact)
- Psychology Interjurisdictional Compact (PSYPACT)
- Audiology and Speech-Language Pathology Interstate Compact (ASLP-IC)
Healthcare organizations should actively track which states participate in relevant compacts and encourage providers to pursue licensure through these pathways when available.
Implementing Credentialing Software Solutions
Technology has a critical role to play in solving telehealth credentialing challenges.
Modern credentialing software platforms offer features specifically designed for telehealth providers:
Cloud-Based Credential Management Systems
These systems serve as central repositories for provider credentials with capabilities including:
- Document storage with OCR functionality
- Automated expiration tracking and reminders
- Primary source verification integration
- Multi-state license management dashboards
API-Enabled Integration
Leading solutions offer API connections that:
- Integrate with state licensing boards for status updates
- Connect with telehealth platforms for real-time credentialing verification
- Link with payer enrollment systems
- Interface with scheduling systems to prevent unauthorized practice
Automated Workflow Management
Workflow automation features can:
- Track application progress across multiple states
- Trigger renewal processes based on jurisdiction-specific timelines
- Generate jurisdiction-specific application forms pre-populated with provider information
- Flag potential issues requiring human intervention
Leveraging Delegated Credentialing
Delegated credentialing arrangements can significantly reduce redundant work when implemented effectively.
Hospital Privileging by Proxy
The Centers for Medicare & Medicaid Services (CMS) allows hospitals to credential and privilege telehealth providers by proxy.
Under this arrangement:
- The distant site (where the telehealth provider is located) completes primary credentialing
- The originating site (where the patient is located) can rely on the distant site’s credentialing process
- The arrangement must be formalized through a written agreement
- Regular information sharing about provider quality must occur
Payer Delegation Agreements
Similarly, payer delegation agreements allow healthcare organizations to:
- Credential providers once within their system
- Have those credentials recognized by participating payers
- Reduce duplicate verification processes
- Accelerate time-to-reimbursement
To implement these strategies effectively, organizations should:
- Develop standardized processes that meet or exceed regulatory requirements
- Create robust quality monitoring systems
- Maintain meticulous documentation
- Pursue formal delegation agreements with key partners
Centralizing Credentialing Operations
For healthcare systems operating across multiple states, centralizing credentialing operations offers significant advantages.
Creating Centers of Excellence
A telehealth credentialing center of excellence consolidates expertise and resources by:
- Building teams with specialized knowledge of state-specific requirements
- Developing standardized processes that accommodate jurisdictional variations
- Creating economies of scale for verification activities
- Establishing consistent quality standards
Standardizing Documentation Requirements
While state requirements vary, organizations can standardize their internal processes by:
- Creating a “universal” documentation package that meets the highest standard across all jurisdictions
- Implementing digital signature solutions that work across states
- Developing standard operating procedures for each state’s unique requirements
- Building comprehensive provider profiles with “always updated” information
Outsourcing to Specialized Telehealth CVOs
As telehealth has grown, specialized Credentialing Verification Organizations have emerged to address its unique challenges.
Benefits of Telehealth-Focused CVOs
These specialized organizations offer:
- Expertise in state-specific telehealth regulations
- Experience with interstate compact applications
- Established relationships with state medical boards
- Dedicated resources for expedited processing
Considerations When Outsourcing
When selecting a telehealth CVO partner, organizations should evaluate:
- Experience with relevant provider types
- Coverage of states where the organization operates
- Integration capabilities with existing systems
- Pricing models and service level agreements
- NCQA certification status
Implementing Continuous Monitoring
Rather than point-in-time credentialing, continuous monitoring offers a more effective approach for telehealth providers.
Real-Time License Monitoring
Continuous monitoring solutions can:
- Track license status changes across multiple states
- Alert organizations to disciplinary actions
- Monitor exclusion databases (OIG, SAM, etc.)
- Track DEA registration status for prescribing providers
Integration with Quality Metrics
Advanced systems link credentialing with quality data:
- Patient satisfaction scores
- Clinical outcomes
- Documentation compliance
- Telehealth-specific metrics (technical proficiency, virtual bedside manner)
Future Directions in Telehealth Credentialing
As telehealth continues to evolve, several emerging trends show promise for further streamlining credentialing processes.
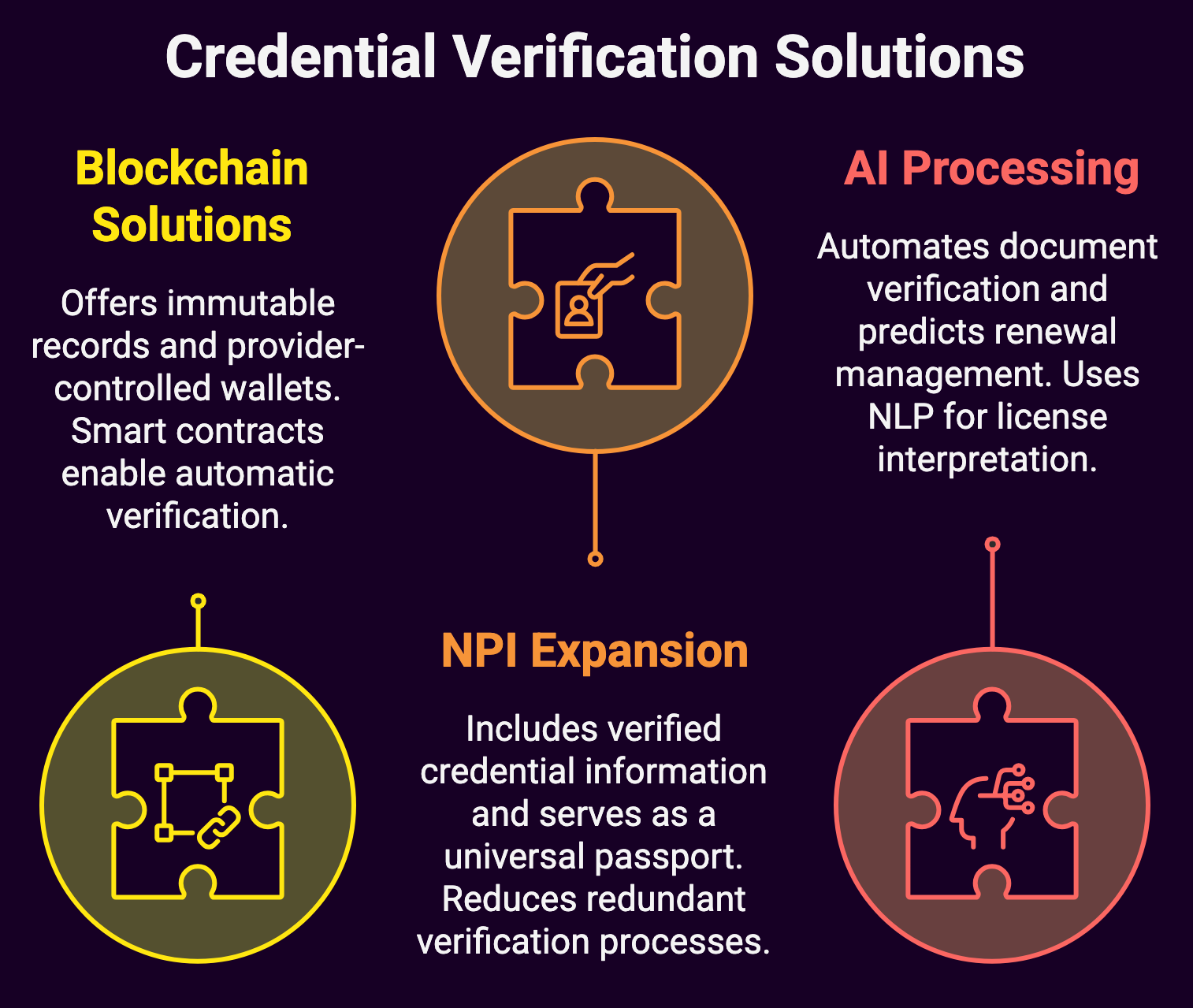
Blockchain for Credential Verification
Blockchain technology offers potential solutions through:
- Immutable, verified credential records
- Provider-controlled digital wallets for credentials
- Smart contracts for automatic verification
- Reduction in primary source verification costs
While still emerging, several pilot programs are testing blockchain-based credentialing systems with promising early results.
National Provider Identifier (NPI) Expansion
Healthcare policy experts have proposed expanding the NPI system to:
- Include verified credential information
- Serve as a universal provider passport
- Reduce redundant verification processes
- Create a single source of truth for basic provider information
Artificial Intelligence in Credential Processing
AI and machine learning are being applied to credentialing challenges through:
- Automated document verification
- Predictive analytics for renewal management
- Natural language processing for license requirement interpretation
- Anomaly detection for potential compliance issues
Building an Effective Telehealth Credentialing Strategy
For healthcare organizations looking to optimize their telehealth credentialing processes, a comprehensive strategy is essential.
Assessing Current State
Begin by thoroughly evaluating:
- Current credentialing timelines and bottlenecks
- Provider satisfaction with existing processes
- Compliance with state-specific requirements
- Resources allocated to telehealth credentialing
Developing a Roadmap
Create a phased implementation plan that:
- Identifies quick wins for immediate efficiency gains
- Maps long-term technological investments
- Establishes clear metrics for success
- Assigns clear ownership for implementation steps
Engaging Key Stakeholders
Successful implementation requires buy-in from:
- Providers who must supply documentation
- Legal teams who ensure regulatory compliance
- Operations leaders who allocate resources
- IT teams who support technology implementation
- Executive sponsors who champion organizational change
Summary: Telehealth Credentialing has Challenges, but They’re Manageable
Telehealth credentialing represents a significant challenge for healthcare organizations, but also an opportunity to develop more efficient, patient-centered processes. Embracing technological solutions, leveraging regulatory innovations, and implementing strategic operational changes, enables healthcare organizations to transform credentialing from a bottleneck to a competitive advantage.
Telehealth will continues to exist as a critical component of healthcare delivery. Hence, organizations that solve the credentialing puzzle will be better positioned to expand their services, attract top provider talent, and ultimately deliver superior care to patients regardless of location. The future of telehealth depends not just on clinical innovation, but on our ability to solve these essential operational challenges.

