Physicians face mounting administrative burdens that contribute significantly to burnout and diminished well-being. Among these burdens, the complex and often repetitive process of medical credentialing stands out as a particular pain point. The current credentialing system is fragmented, redundant, and time-intensive and it takes physicians away from patient care and adds unnecessary stress to their professional lives. Revamping credentialing applications and processes can support physician well-being while maintaining the necessary safeguards for quality care.
The Current State of Credentialing: A Well-Being Challenge
 Medical credentialing serves the essential purpose of verifying that healthcare providers possess the qualifications, training, and clean record necessary to deliver safe, high-quality care. However, the implementation of this necessary function has evolved into a labyrinthine process that places excessive demands on physicians’ time and mental resources.
Medical credentialing serves the essential purpose of verifying that healthcare providers possess the qualifications, training, and clean record necessary to deliver safe, high-quality care. However, the implementation of this necessary function has evolved into a labyrinthine process that places excessive demands on physicians’ time and mental resources.
The typical physician maintains privileges at multiple healthcare facilities and participates in numerous insurance networks, each with its own credentialing application and renewal timeline. Despite collecting largely identical information, these entities rarely coordinate their processes, leading to significant duplication of effort. Physicians must repeatedly provide the same information, education history, training details, work experience, licensing data, and more, in slightly different formats to meet each organization’s requirements.
The numbers tell a sobering story. Physicians spend an average of 3-4 hours completing each credentialing application, with many completing 10-20 applications per year. This translates to potentially 40-80 hours annually (the equivalent of one to two full work weeks) devoted solely to credentialing paperwork. For physicians already working 50-60 hours weekly on direct patient care and other administrative tasks, this additional burden can tip the scales toward burnout.
Beyond the time commitment, credentialing processes create significant cognitive load through:
- Tracking multiple application deadlines and renewal cycles
- Maintaining current copies of numerous documents (licenses, certifications, CME records)
- Remembering details from training programs completed decades ago
- Navigating different online portals and interfaces
- Responding to repetitive verification requests and follow-up questions
The psychological impact extends beyond mere annoyance. The persistent demand to document and re-document qualifications can feel undermining to physicians who have dedicated years to training and practice. The implicit message (that their professional standing must be repeatedly justified) conflicts with their sense of professional identity and autonomy.
The Well-Being Impact: Beyond Frustration
The effects of burdensome credentialing processes on physician well-being are multifaceted and significant. Research has consistently identified administrative burden as a leading contributor to physician burnout, with credentialing representing a substantial component of that burden.
At the most basic level, credentialing demands consume limited time resources, contributing to work-life imbalance and reducing time available for self-care activities that support well-being. When physicians must complete credentialing paperwork during evenings and weekends, as is often the case, personal and family time suffers.
The cognitive challenges of credentialing also take a toll. The task-switching required to move between clinical work and administrative paperwork creates mental fatigue. The anxiety of potentially missing deadlines or providing incomplete information adds another layer of stress. For physicians who practice across state lines or in multiple facilities, these challenges multiply.
Perhaps most concerning is the demoralizing effect of redundant bureaucracy. Physicians enter medicine motivated by a desire to help patients and apply their clinical skills. Being repeatedly pulled away from this core purpose to complete paperwork that seems disconnected from patient care reinforces cynicism and diminishes professional satisfaction.
These well-being impacts extend beyond individual physicians to affect healthcare organizations and patients. Burned-out physicians are more likely to reduce their clinical hours, leave practice entirely, or make medical errors. By contributing to burnout, inefficient credentialing processes indirectly undermine the very quality and safety standards they aim to uphold.
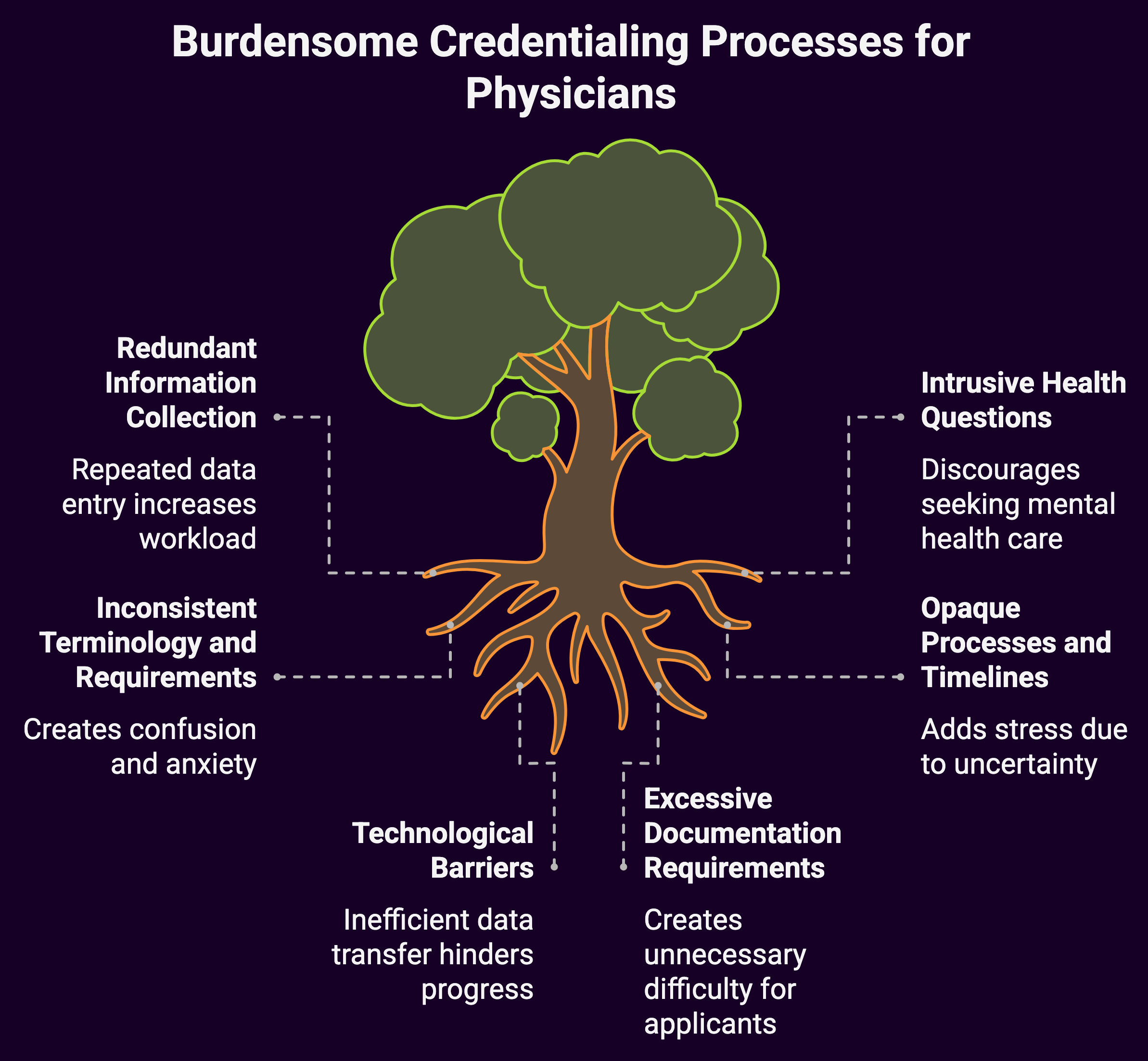
Specific Pain Points in Current Credentialing Applications
To effectively revamp credentialing to support well-being, we must first identify the specific elements of current applications and processes that create unnecessary burden:
Redundant Information Collection
The most obvious issue is the redundancy across applications. Physicians must repeatedly provide basic information. Name, demographics, education, training history. That rarely changes. The same verification processes occur in parallel across multiple organizations, with each independently contacting the same primary sources.
Intrusive Health Questions
Many credentialing applications include questions about physical and mental health history that are overly broad and potentially discriminatory. Questions like “Have you ever been treated for a mental health condition?” create a chilling effect that discourages physicians from seeking needed mental health care for fear of credentialing consequences.
Inconsistent Terminology and Requirements
Variation in how different organizations define terms like “disciplinary action,” “investigation,” or “impairment” creates confusion and anxiety. A minor issue that requires disclosure on one application might not need reporting on another, forcing physicians to make difficult judgment calls with potentially serious consequences.
Opaque Processes and Timelines
Many credentialing systems provide little transparency regarding application status, expected processing times, or reasons for delays. This uncertainty adds unnecessary stress, particularly when income depends on completing the credentialing process.
Technological Barriers
Despite advances in digital technology, many credentialing systems still rely on outdated interfaces, paper forms, or non-interoperable electronic systems. Physicians must often manually re-enter the same information across multiple platforms rather than being able to transfer data efficiently.
Excessive Documentation Requirements
Requirements to provide documentation for activities from the distant past, such as detailed case logs from residency or exact dates of short-term locum tenens positions from years ago—create disproportionate difficulty relative to their value in assessing current competence.
A Better Approach: Principles for Well-Being-Conscious Credentialing
Reimagining credentialing with physician well-being in mind doesn’t mean abandoning the essential function of verifying qualifications. Rather, it means designing systems that accomplish this necessary goal while minimizing unnecessary burden.
Several key principles should guide this effort:
Collect Once, Use Many Times
The cornerstone of well-being-conscious credentialing is eliminating redundancy. Information that rarely changes. Stuff like education history, training details, past employment should be collected once and shared across organizations with physician consent. This approach, sometimes called the “passport model,” allows organizations to focus verification efforts on new information rather than repeatedly checking the same credentials.
Standardize Requirements and Terminology
Creating consistent definitions and requirements across credentialing bodies would reduce confusion and simplify compliance. Standardized forms, with identical questions and formats, would allow physicians to maintain a single set of responses that could be submitted to multiple organizations.
Focus on Relevant Information
Credentialing should focus on information that directly relates to a physician’s ability to provide safe, quality care in their specific practice context. Historical information that has minimal bearing on current competence should be de-emphasized or eliminated from regular recredentialing processes.
Ensure Appropriate Health Questions
Questions about physician health should focus narrowly on current impairment that affects the ability to practice safely, not on diagnoses or past treatment. This approach aligns with legal requirements under the Americans with Disabilities Act while encouraging physicians to seek appropriate healthcare without fear of credentialing consequences.
Embrace Technology Thoughtfully
Technology should serve as an enabler of simplification rather than an additional barrier. Digital systems should feature intuitive interfaces, pre-population of known information, interoperability between platforms, and secure data sharing capabilities.
Provide Transparency and Support
Credentialing systems should offer clear timelines, status updates, and support resources. Physicians should have access to knowledgeable staff who can answer questions and provide guidance on complex aspects of the process.
Promising Models and Innovations
Several models and initiatives demonstrate how credentialing can be redesigned to reduce burden while maintaining quality standards:
Federation Credentials Verification Service (FCVS)
Operated by the Federation of State Medical Boards, FCVS creates a permanent, lifetime repository for a physician’s core credentials that can be shared with state licensing boards. This model demonstrates the feasibility of verified credential repositories, though its scope remains limited to state licensing rather than facility credentialing or payer enrollment.
Council for Affordable Quality Healthcare (CAQH) ProView
The CAQH ProView system allows physicians to enter their information once into a standard form that can then be shared with multiple health plans. While not entirely complete, this system has demonstrated significant time savings for participating providers and plans. We’ve built a CAQH ProView Form in order to capture all variables and make this easier on providers and groups, for their application process.
State Streamlining Initiatives
Several states have enacted legislation to standardize credentialing processes and timelines across payers. These “Any Willing Provider” or “Clean Credentialing Application” laws typically establish maximum processing times and standard information requirements, reducing uncertainty and variation.
Regional Centralized Verification Organizations
Some healthcare markets have developed regional Credentials Verification Organizations (CVOs) that perform primary source verification for multiple facilities within a geographic area. This collaborative approach reduces duplication while maintaining appropriate oversight.
Blockchain and Digital Credential Technologies
Emerging technologies offer new possibilities for secure, verifiable digital credentials that could dramatically streamline verification processes. Blockchain-based systems that create permanent, tamper-proof records of credentials could potentially eliminate the need for repeated primary source verification.
Implementation Path: From Concept to Reality
Transforming credentialing to support physician well-being requires coordinated action across multiple stakeholders:
Healthcare Organizations
Hospitals and health systems can take immediate steps to evaluate and streamline their credentialing processes, including:
- Conducting time-motion studies to identify specific pain points
- Eliminating requirements that exceed regulatory minimums
- Implementing technology that reduces manual data entry
- Creating “fast track” processes for recredentialing providers in good standing
- Coordinating credentialing across affiliated facilities
Health Plans and Payers
Insurers and managed care organizations can contribute by:
- Participating in standardized provider data systems like CAQH ProView
- Accepting hospital verification for shared data elements
- Implementing delegated credentialing arrangements with high-quality provider organizations
- Providing transparent timelines and status updates
Medical Associations
Professional societies play a crucial advocacy role and can:
- Continue pushing for legislative reforms that standardize processes
- Develop consensus-based standards for appropriate health questions
- Create educational resources to help physicians navigate credentialing efficiently
- Partner with technology providers to design physician-friendly systems
Regulatory Bodies and Accreditors
Organizations like state licensing boards, The Joint Commission, and the National Committee for Quality Assurance can support well-being through:
- Harmonizing requirements to reduce unnecessary variation
- Focusing on outcomes rather than process documentation
- Explicitly considering administrative burden when developing new standards
- Supporting innovations in credential verification methods
Individual Physicians
Physicians themselves can contribute to solutions by:
- Documenting specific pain points in current systems
- Participating in pilot programs for new approaches
- Advocating through professional societies and governance roles
- Implementing personal systems to organize credentialing information
The Business Case for Change
Beyond the ethical imperative to support physician well-being, there are compelling business reasons to invest in credentialing reform.
The current system imposes significant costs on all stakeholders:
- Physicians lose productive time that could be spent on patient care or personal wellness
- Healthcare organizations maintain expensive credentialing departments and face delays in bringing new providers onto staff
- Health plans incur administrative costs for maintaining separate verification processes
- The healthcare system as a whole bears the costs of physician burnout, turnover, and reduced productivity
Industry analyses suggest that streamlining credentialing could save billions annually across the healthcare system while simultaneously improving provider satisfaction and retention.
Summary: A Call for Coordinated Action
![]()
Revamping credentialing applications and processes represents a tangible opportunity to reduce administrative burden and support physician well-being. Unlike many contributors to burnout that involve complex system redesign, credentialing inefficiencies can be addressed through practical, incremental changes that yield immediate benefits.
The path forward requires balancing multiple priorities: protecting patient safety, meeting regulatory requirements, controlling costs, and supporting physician well-being. Credentialing can go from a burdensome obstacle to an efficient, streamlined function that serves its essential purpose without unnecessary burden.
Physicians, patients, and healthcare organizations all stand to benefit from a credentialing system that maintains high standards while respecting the finite time and mental resources of the clinicians it aims to verify.

