Provider credentialing stands as a critical yet often challenging process that healthcare organizations must navigate effectively. Below, we address the fundamental questions surrounding credentialing while offering practical strategies to streamline operations, reduce turnaround times, and maintain regulatory compliance.
Understanding the Provider Credentialing Process
Provider credentialing is the systematic verification of a healthcare provider’s qualifications, including education, training, licensure, certifications, and practice history. This meticulous process serves as the foundation for patient safety, quality care, and organizational integrity. Though essential, credentialing often becomes a significant administrative burden, consuming valuable resources and potentially delaying provider onboarding.
Why Is Credentialing So Important?
Credentialing serves multiple critical functions within healthcare organizations:
- Patient Safety and Quality Assurance: By verifying provider qualifications, organizations ensure that only competent professionals deliver patient care.
- Regulatory Compliance: Healthcare facilities must adhere to strict regulations from accrediting bodies like The Joint Commission, NCQA, and state licensing boards.
- Financial Stability: Proper credentialing enables accurate billing and reimbursement from insurance payers, directly impacting revenue cycles.
- Risk Management: Thorough credentialing processes help mitigate liability risks associated with negligent credentialing claims.
- Reputation Management: Organizations with robust credentialing procedures demonstrate commitment to excellence and patient safety.
Key Challenges in Provider Credentialing
Despite its importance, several obstacles make credentialing particularly challenging:
1. Lengthy Turnaround Times
The traditional credentialing process can take anywhere from 60 to 180 days, significantly delaying provider onboarding and potentially affecting:
- Revenue generation
- Provider satisfaction
- Patient access to care
- Competitive advantage in provider recruitment
2. Complex Documentation Requirements
Providers must supply numerous documents, including but not limited to:
- Medical school diplomas
- Residency and fellowship certificates
- State medical licenses
- DEA registrations
- Board certifications
- Professional liability insurance
- Continuing medical education records
- Work history and references
- Hospital privileges documentation
3. Variation in Payer Requirements
Each insurance payer maintains unique credentialing requirements, application forms, and verification procedures, creating a complex web of administrative tasks.
4. Ongoing Monitoring and Recredentialing
Credentialing isn’t a one-time process. Organizations must continuously monitor provider status and complete recredentialing every 2-3 years, tracking expiration dates for numerous credentials.
Essential Questions About Provider Credentialing
What is the difference between credentialing and privileging?
While often mentioned together, these processes serve distinct purposes:
- Credentialing verifies a provider’s qualifications and competency through documentation review, including education, training, licensure, and practice history.
- Privileging determines the specific clinical activities a provider may perform within a particular healthcare facility based on their demonstrated competence, training, and experience.
Think of credentialing as establishing a provider’s baseline qualifications, while privileging defines their specific authorized scope of practice at your facility.
How long does the credentialing process typically take?
The credentialing timeline varies considerably based on several factors:
- Traditional paper-based processes: 90-180 days
- Optimized digital workflows: 30-60 days
- Urgent/temporary privileges: 7-14 days (in special circumstances)
Factors affecting turnaround time include:
- Completeness of provider applications
- Responsiveness of verification sources
- Number of privileges requested
- Committee meeting schedules
- Payer processing times
- Organizational workflow efficiency
- Technology utilization
What documentation is required for provider credentialing?
The comprehensive documentation required typically includes:
Personal Information:
- Full legal name and any name variations
- Contact information
- NPI number
- Social Security Number
- Date of birth
- Citizenship/visa status
Education and Training:
- Medical/professional school diploma
- Residency completion certificate
- Fellowship documentation
- Specialty training verification
Licensure and Certifications:
- State medical/professional license
- DEA registration
- Board certification documentation
- ECFMG certification (for international graduates)
- CPR/ACLS/PALS certifications (if applicable)
Practice History:
- Work history (typically 5-10 years without gaps)
- Clinical references (usually 3-5 professional peers)
- Peer evaluations
Additional Documentation:
- Professional liability insurance coverage
- Claims history/malpractice experience
- Health status attestation
- Immunization records
- Background check authorization
- Sanction and exclusion checks (OIG, GSA, NPDB)
- Continuing education documentation
What can cause delays in the credentialing process?
Several common factors contribute to credentialing delays:
- Incomplete applications: Missing information or documentation is the leading cause of delays, affecting up to 80% of applications.
- Provider responsiveness: Delayed responses to additional information requests significantly extend timelines.
- Primary source verification challenges: Difficulty obtaining timely responses from education institutions, previous employers, or reference contacts.
- Committee scheduling: Credential committee meetings that occur infrequently (monthly or quarterly) can create bottlenecks.
- Manual workflows: Paper-based processes with manual verification steps introduce inefficiencies and errors.
- Payer-specific requirements: Navigating the unique requirements of multiple insurance payers adds complexity.
- Staff experience and workload: Credentialing specialists with heavy workloads or limited experience may struggle with complex cases.
- International verification challenges: Verifying credentials from foreign institutions often involves additional steps and longer response times.
What are the consequences of credentialing errors or delays?
The impact of credentialing inefficiencies extends throughout healthcare organizations:
Financial Impact:
- Revenue loss ranging from $7,000 to $50,000 per physician per month of delay
- Payer claim denials for services provided by improperly credentialed providers
- Potential fines for regulatory non-compliance
- Additional administrative costs for rework and expedited processing
Operational Impact:
- Delayed provider start dates
- Scheduling disruptions
- Increased administrative workload
- Resource reallocation to address bottlenecks
Strategic Impact:
- Competitive disadvantage in provider recruitment
- Potential loss of qualified candidates to competitors
- Reduced patient access to care
- Provider dissatisfaction affecting retention
Legal and Compliance Risks:
- Potential for negligent credentialing claims
- Regulatory violations
- Accreditation challenges
- Patient safety concerns
Strategies to Streamline the Credentialing Process
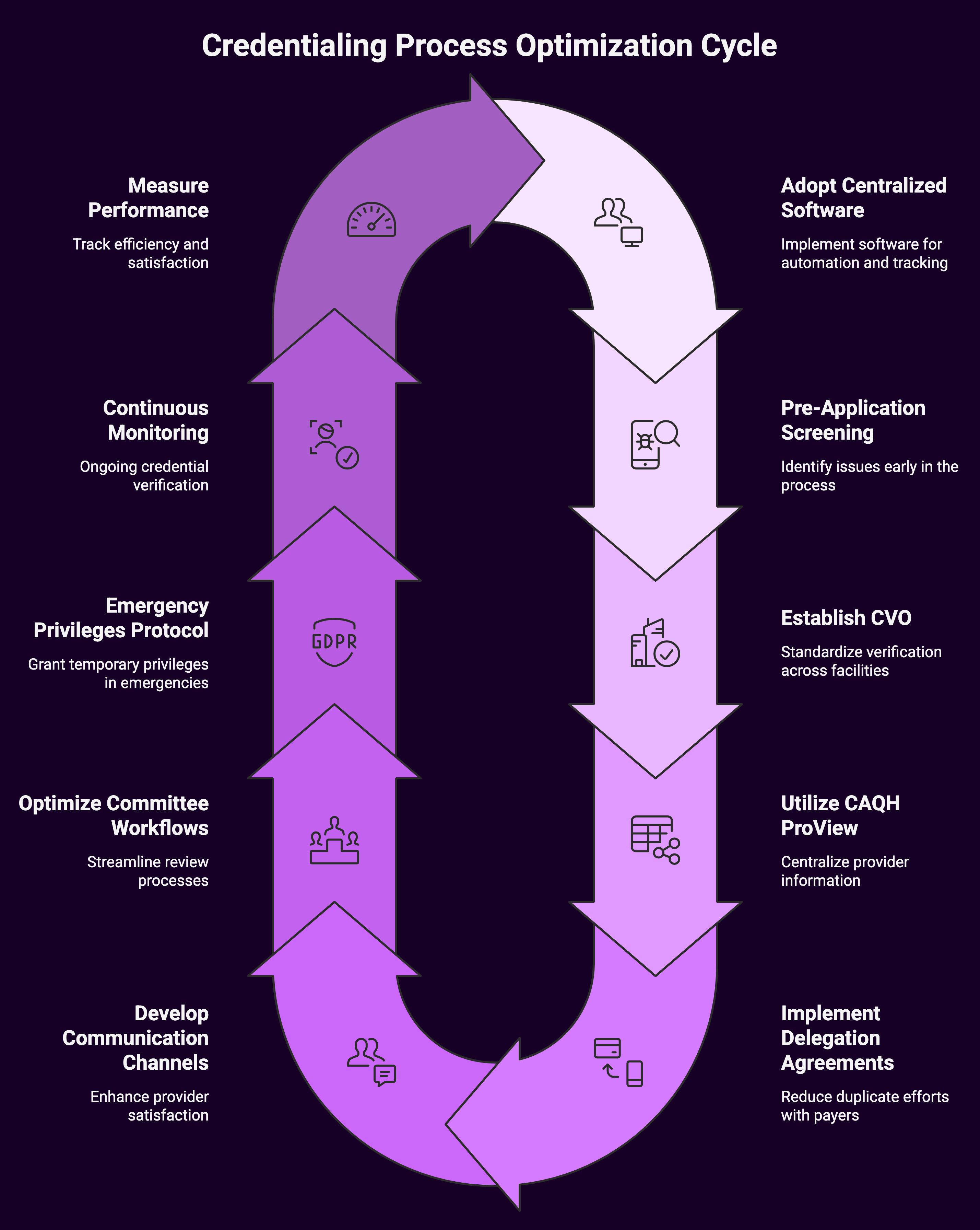
Implementing effective strategies can significantly improve credentialing efficiency:
1. Adopt Centralized Credentialing Software
Modern credentialing systems offer substantial benefits:
- Automated primary source verification
- Digital application submission and tracking
- Customizable workflows with automated reminders
- Integrated background screening
- Real-time status monitoring
- Comprehensive reporting capabilities
- Document expiration tracking and alerts
- Integration with enrollment and privileging processes
Organizations implementing comprehensive credentialing software report:
- 50-70% reduction in processing time
- 40-60% decrease in administrative costs
- Significant improvement in accuracy rates
- Enhanced provider satisfaction
2. Implement Pre-Application Screening
Proactive screening before formal application submission helps identify potential issues early:
- Verify licensure status and restrictions
- Check OIG/SAM exclusion lists
- Review National Practitioner Data Bank reports
- Confirm basic eligibility requirements
- Identify potential red flags requiring additional review
This approach prevents investing resources in applications unlikely to meet organizational requirements.
3. Establish a Credentialing Verification Organization (CVO)
For larger healthcare systems, establishing an internal CVO creates economies of scale:
- Standardized verification processes across multiple facilities
- Consolidated expertise and resources
- Reduced duplication of verification efforts
- Consistent quality control measures
- Streamlined payer enrollment coordination
4. Utilize CAQH ProView
The Council for Affordable Quality Healthcare (CAQH) ProView system serves as a centralized repository for provider information:
- Providers maintain a single, comprehensive profile
- Organizations access standardized data for credentialing
- Regular attestation ensures data currency
- Reduced redundant data entry for providers
- Streamlined primary source verification
Over 1.4 million providers and most major health plans now utilize CAQH ProView, making it an industry standard.
5. Implement Delegation Agreements
Delegation agreements with payers allow healthcare organizations to credential providers once, with payers accepting those credentials:
- Significant reduction in duplicate efforts
- Faster payer enrollment timelines
- Lower administrative burden
- Potential for earlier reimbursement eligibility
While beneficial, delegation requires organizations to maintain rigorous compliance with payer standards and undergo regular audits.
6. Develop Clear Communication Channels
Transparent provider communication throughout the credentialing process improves satisfaction and efficiency:
- Comprehensive application instructions
- Clearly defined documentation requirements
- Regular status updates
- Single point of contact for questions
- Online portals for document submission and tracking
- Timeline expectations
- Proactive notification of potential issues
7. Optimize Committee Workflows
Streamlining committee review processes reduces bottlenecks:
- Implement clear criteria for expedited reviews
- Increase committee meeting frequency
- Utilize virtual review options for routine cases
- Develop consistent evaluation criteria
- Pre-review materials distribution to committee members
- Establish clear approval pathways based on provider type
8. Develop an Emergency Privileges Protocol
Create a clearly defined process for granting temporary privileges during urgent situations while maintaining compliance:
- Minimum verification requirements
- Time limitations on temporary privileges
- Required oversight and monitoring
- Documentation of rationale
- Process for converting to permanent privileges
- Regular reporting to the credentials committee
9. Implement Continuous Monitoring
Rather than periodic credential verification, implement ongoing monitoring systems:
- License status monitoring
- Sanction and exclusion screening
- Malpractice claim alerts
- Board certification tracking
- DEA registration monitoring
Continuous monitoring helps identify issues between formal recredentialing cycles, enhancing patient safety and compliance.
10. Measure and Optimize Performance
Implement key performance indicators to track credentialing efficiency:
- Average turnaround time (overall and by provider type)
- Application completion rate
- First-pass approval percentage
- Provider satisfaction scores
- Error and rework rates
- Cost per application processed
- Verification response times
Regular analysis of these metrics helps identify bottlenecks and opportunities for process improvement.
The Future of Provider Credentialing
Several emerging trends are reshaping credentialing processes:
Blockchain Technology
Blockchain solutions offer promising applications for credentialing:
- Immutable verification of credentials
- Reduced need for repetitive primary source verification
- Provider-controlled digital credential wallets
- Transparent audit trails
- Enhanced security and fraud prevention
Artificial Intelligence and Machine Learning
AI technologies are increasingly integrated into credentialing workflows:
- Predictive analytics for application completeness
- Automated document verification
- Pattern recognition for fraud detection
- Intelligent workflow routing
- Risk scoring for prioritization
Interstate Licensure Compacts
The growing adoption of interstate licensure compacts facilitates multistate practice:
- Interstate Medical Licensure Compact (IMLC)
- Nurse Licensure Compact (NLC)
- Psychology Interjurisdictional Compact (PSYPACT)
- Physical Therapy Compact (PT Compact)
These agreements streamline credentialing for providers practicing across state lines, particularly for telehealth services.
Summary: Building a Sustainable Credentialing Strategy
An effective credentialing strategy balances efficiency, compliance, and provider satisfaction.
Organizations should:
- Assess current processes to identify bottlenecks and inefficiencies
- Invest in appropriate technology based on organizational size and complexity
- Standardize procedures across the organization
- Train credentialing staff on best practices and regulatory requirements
- Engage providers as partners in the credentialing process
- Establish clear metrics to measure success
- Continuously improve based on performance data and feedback
Healthcare organizations can transform credentialing from an administrative burden into a strategic advantage. They can enhance provider recruitment, accelerate revenue cycles, and ultimately improve patient care. Provider credentialing, while complex, need not be overwhelming. With the right approach, organizations can achieve significant improvements in efficiency while maintaining the rigorous standards essential for quality healthcare delivery.

