Provider credentialing represents one of healthcare administration’s most significant bottlenecks. This essential but often frustrating process verifies a healthcare provider’s qualifications, competencies, and practice history before they can join a healthcare organization or insurance network.
When delays occur, everyone suffers. Providers face income loss, healthcare organizations struggle with staffing shortages, and patients experience limited access to care.
The traditional credentialing process can take anywhere from 60 to 180 days, causing substantial revenue loss and operational challenges. However, with strategic planning, technology adoption, and process optimization, these delays can be significantly reduced. Within the following content, we look at a number of strategies to streamline the provider credentialing process and prevent unnecessary delays.
Understanding the Credentialing Process
Before diving into prevention strategies, it’s important to understand what makes credentialing so time-consuming.
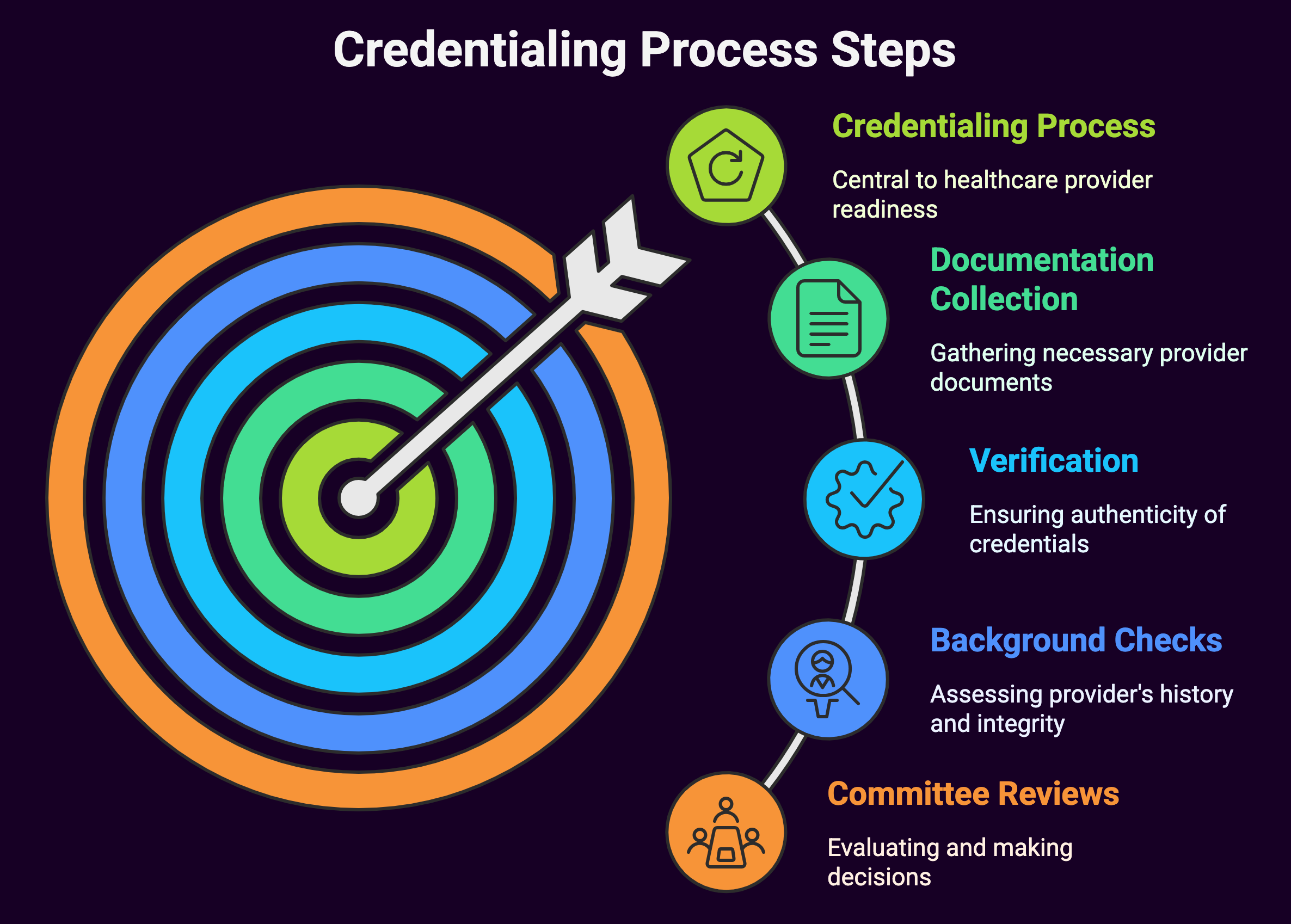
The process typically involves:
- Collecting extensive documentation from providers
- Primary source verification of education, training, licensure, and work history
- Background checks and sanctions screening
- Committee reviews and decision-making
- Insurance carrier enrollment
- Hospital privileging
- State-specific requirements compliance
Each step introduces potential for delay, especially when managed through outdated manual systems or when faced with incomplete information. Let’s examine how to address these challenges systematically.
Proactive Planning and Application Management
Begin Early

The single most effective way to prevent credentialing delays is to start the process as early as possible. Ideally, credentialing should begin 120-180 days before a provider’s anticipated start date. For graduating residents or fellows, this means initiating the process during their final year of training.
Healthcare organizations should establish clear timelines that account for each step of the credentialing process, including buffer time for unexpected delays. These timelines should be communicated clearly to all new providers during the recruitment process so they understand the importance of prompt document submission.
Create a Pre-Application Process
Implementing a pre-application screening can identify potential issues before the formal credentialing process begins.
This preliminary step can save significant time by addressing red flags early, such as:
- Gaps in work history
- Pending investigations or actions against licenses
- Expired certifications
- Immigration or visa status issues
- State-specific requirements
Addressing these concerns proactively prevents the stop-and-start pattern that frequently delays credentialing.
Develop Comprehensive Application Packets
One major source of delay is incomplete applications.
Create detailed application packets that include:
- Clear instructions for each form
- Checklists of required documents
- Examples of properly completed forms
- Contact information for questions
- Digital submission options
Consider implementing a provider portal where applicants can access these materials, track their progress, and receive automated reminders about missing information.
Optimize Internal Workflows
Standardize and Document Processes
Many credentialing delays stem from inconsistent internal processes.
Develop standardized procedures for each step of the credentialing workflow, including:
- Document collection protocols
- Verification procedures
- Committee review schedules
- Approval pathways
- Communication templates
These documented workflows should be accessible to all team members involved in credentialing and updated regularly to reflect changing requirements.
Implement Batch Processing
Rather than handling applications one at a time, consider implementing batch processing for similar tasks. For example, schedule dedicated time for all primary source verifications, committee reviews, or payer enrollments. This approach reduces context switching and improves focus and efficiency.
Establish Regular Committee Meetings
Credentialing committee meetings that occur infrequently or are frequently rescheduled create significant bottlenecks. Establish a regular meeting schedule with alternative members who can step in when primary members are unavailable. Consider implementing a virtual review option for straightforward cases that don’t require extensive discussion.
Develop Parallel Processing Capabilities
Not all credentialing steps need to happen sequentially. Identify steps that can occur simultaneously and restructure your workflow accordingly. For example, hospital privileging applications can often proceed alongside payer enrollment processes.
Leverage Technology Solutions
Implement Credentialing Software
Modern credentialing software represents one of the most impactful investments for preventing delays.
These platforms offer:
- Centralized data management
- Automated workflow tracking
- Document expiration monitoring
- Integration with verification sources
- Electronic signature capabilities
- Reporting and analytics features
The right credentialing software can dramatically reduce processing time and minimize human error. When selecting a platform, prioritize user-friendliness, integration capabilities, and robust security features.
Automate Verification Processes
Primary source verification traditionally consumes substantial staff time.
Many verification organizations now offer electronic interfaces that can drastically reduce this burden:
- Medical schools and residency programs increasingly provide digital verification services
- State licensing boards offer API connections for real-time verification
- The National Practitioner Data Bank provides batch query capabilities
- Background check services can integrate directly with credentialing systems
Each automated verification point eliminates days or weeks from the traditional process.
Implement Digital Document Management
Paper documents and manual filing systems introduce numerous opportunities for delay.
Implement a digital document management system with features like:
- Secure document upload capabilities
- Automatic file organization
- OCR technology for searchable documents
- Version control
- Permission-based access
- Audit trails
Digital systems eliminate physical transfer time and reduce the risk of documents being lost or misfiled.
Enhance Communication and Transparency
Establish Clear Communication Channels
Poor communication frequently exacerbates credentialing delays.
Designate specific communication channels and points of contact for each stakeholder in the process:
- Assign each provider a dedicated credentialing specialist
- Create provider-facing status dashboards
- Schedule regular check-in calls during the process
- Establish escalation pathways for urgent issues
- Implement automated status updates
Clear communication reduces anxiety, prevents duplicative work, and enables faster problem resolution.
Create Transparency Through Tracking Systems
Implement tracking systems that provide real-time visibility into the credentialing process.
These systems should allow providers and administrators to see:
- Current application status
- Outstanding documentation needs
- Anticipated completion dates
- Bottlenecks or delays
- Next steps and responsibilities
This transparency helps manage expectations and enables proactive problem-solving.
Develop Service Level Agreements
Establish internal service level agreements (SLAs) for each step of the credentialing process.
These SLAs should define:
- Maximum processing times for each stage
- Response time expectations for inquiries
- Escalation thresholds
- Performance metrics and reporting cadence
Regular review of SLA performance helps identify and address systemic issues before they cause widespread delays.
Build Strategic Partnerships
Strengthen Relationships with Verification Sources
Building relationships with frequent verification sources can expedite the process significantly.
Consider:
- Establishing direct contacts at key medical schools, training programs, and hospitals
- Creating memoranda of understanding with state licensing boards
- Joining verification networks or consortiums
- Participating in industry standardization efforts
These relationships can provide priority processing and alert you to changing requirements.
Utilize Credentials Verification Organizations (CVOs)
CVOs specialize in primary source verification and often maintain extensive databases of pre-verified information.
Working with reputable CVOs can:
- Reduce duplication of verification efforts
- Provide access to specialized verification expertise
- Decrease processing time for complex verifications
- Create economies of scale
- Offer after-hours processing capabilities
When selecting a CVO, evaluate their accreditation status, turnaround times, and integration capabilities with your systems.
Engage with Professional Organizations
Professional organizations often provide resources that can help prevent credentialing delays:
- Standardized application forms
- Industry best practices
- Educational resources for providers and staff
- Advocacy for regulatory improvements
- Networking with peers facing similar challenges
Active engagement with these organizations helps your team stay informed about emerging solutions and regulatory changes.
Implement Quality Control Measures
Perform Regular Audits
Regular auditing of credentialing processes helps identify inefficiencies and prevent systemic delays.
Schedule quarterly audits that examine:
- Average processing times by stage
- Common reasons for delays
- Compliance with documented procedures
- Data accuracy and completeness
- Staff performance against SLAs
Use audit findings to implement targeted improvements and track their impact over time.
Develop Key Performance Indicators
Establish clear KPIs for your credentialing process that align with organizational goals:
- Average time to credential completion
- Percentage of applications completed within target timeframes
- Error rates requiring rework
- Provider satisfaction scores
- Revenue impact metrics
Monitor these KPIs through regular reporting and discuss them in team meetings to maintain focus on continuous improvement.
Implement Peer Review
Create a peer review system where credentialing specialists periodically review each other’s work.
This approach:
- Identifies individual training needs
- Spreads best practices across the team
- Creates backup knowledge for staff absences
- Increases consistency in application processing
- Builds team accountability
Peer review should be structured as a constructive process focused on improvement rather than criticism.
Optimize Provider Engagement
Provide Comprehensive Onboarding for New Providers
Many credentialing delays occur because providers don’t understand the importance or complexity of the process.
Develop comprehensive onboarding materials that:
- Explain the credentialing timeline and requirements
- Highlight common pitfalls and how to avoid them
- Clarify the provider’s responsibilities
- Introduce key contacts and resources
- Set clear expectations about response times
Consider creating video tutorials or interactive guides that make the information more accessible and engaging.
Implement a Provider Portal
A dedicated provider portal streamlines document submission and communication.
Effective portals include:
- Secure document upload functionality
- Auto-save capabilities for partially completed forms
- Progress tracking and status updates
- Notification systems for pending deadlines
- Message centers for questions and clarifications
- Mobile accessibility for providers on the go
Well-designed portals dramatically reduce the administrative burden on providers while improving document quality and submission timeliness.
Create Provider Education Resources
Develop targeted educational resources that help providers navigate the credentialing process:
- Frequently asked questions documents
- Step-by-step guides for complex requirements
- State-specific requirement summaries
- Checklists for different provider types
- Sample documents and completion guides
These resources should be easily accessible and regularly updated to reflect changing requirements.
Manage Regulatory Compliance Proactively
Monitor Changing Requirements
Regulatory requirements for credentialing change frequently.
Establish a systematic approach to monitoring and implementing these changes:
- Assign staff responsibility for tracking regulatory updates
- Subscribe to relevant newsletters and alerts
- Participate in industry forums and webinars
- Schedule regular reviews of accreditation standards
- Create a change management process for implementation
This proactive approach prevents delays caused by unexpected requirement changes.
Develop State-Specific Expertise
For organizations operating across multiple states, variations in requirements can cause significant delays.
Develop state-specific expertise through:
- State-specific procedure manuals
- Dedicated specialists for high-volume states
- Relationship building with state regulatory bodies
- Regular training on state requirement changes
- Customized application materials by state
This specialized knowledge reduces errors and rework caused by misunderstanding state variations.
Maintain Accreditation Standards
Maintaining relevant accreditations (such as NCQA, URAC, or Joint Commission) ensures your credentialing process meets industry standards.
These accreditations:
- Provide structured frameworks for process improvement
- Demonstrate quality to providers and partners
- Offer access to best practices and benchmarking
- Create accountability for maintaining standards
- May streamline delegated credentialing arrangements
Regular preparation for accreditation reviews helps identify and address potential bottlenecks before they cause widespread delays.
Summary: Avoid Credentialing Delays Through Commonsensical Performance
Preventing delays in the provider credentialing process requires a multifaceted approach combining strategic planning, technology implementation, workflow optimization, and stakeholder engagement. Addressing each potential delay point systematically permits healthcare organizations to transform credentialing from a frustrating bottleneck to a streamlined operational strength.
The most successful credentialing programs combine high-tech solutions with high-touch service, recognizing that while automation drives credentialing efficiency, the human elements of communication and relationship building remain essential. Regulatory requirements aren’t going anywhere and they’re becoming increasingly more complex. Hence, organizations that invest in credentialing excellence gain significant competitive advantages in provider recruitment, retention, and satisfaction.
Healthcare organizations can dramatically reduce credentialing timelines, improve provider satisfaction, minimize revenue loss, and ultimately enhance patient access to care by taking the aforementioned strategies into account. Making the investment in credentialing improvements is a win for all stakeholders.

