Remember the days when medical credentialing meant endless stacks of paperwork, countless phone calls, and weeks (or months) of waiting? For many healthcare administrators, those memories are still all too fresh. But thanks to artificial intelligence, the landscape of medical credentialing is undergoing a dramatic transformation. Let’s dive into how AI is revolutionizing credentialing. A critical yet often overlooked aspect of healthcare administration.
The Traditional Credentialing Headache
 Before we explore the AI revolution, let’s acknowledge the elephant in the room: traditional credentialing is a pain. Just ask Micah Schultz, a credentialing specialist at a large medical group in Boston. “Before we implemented AI-assisted credentialing,” he shares, “I spent roughly 80% of my workday just chasing down documents and verifying information. It was like being a detective, but with much more paperwork.”
Before we explore the AI revolution, let’s acknowledge the elephant in the room: traditional credentialing is a pain. Just ask Micah Schultz, a credentialing specialist at a large medical group in Boston. “Before we implemented AI-assisted credentialing,” he shares, “I spent roughly 80% of my workday just chasing down documents and verifying information. It was like being a detective, but with much more paperwork.”
He’s not alone. The average credentialing process traditionally takes anywhere from 60 to 120 days, costing healthcare organizations both time and money. With each day of delay potentially representing thousands in lost revenue, the stakes are high.
Enter Artificial Intelligence
AI isn’t just changing the game; it’s completely rewriting the rulebook.
Here’s how:
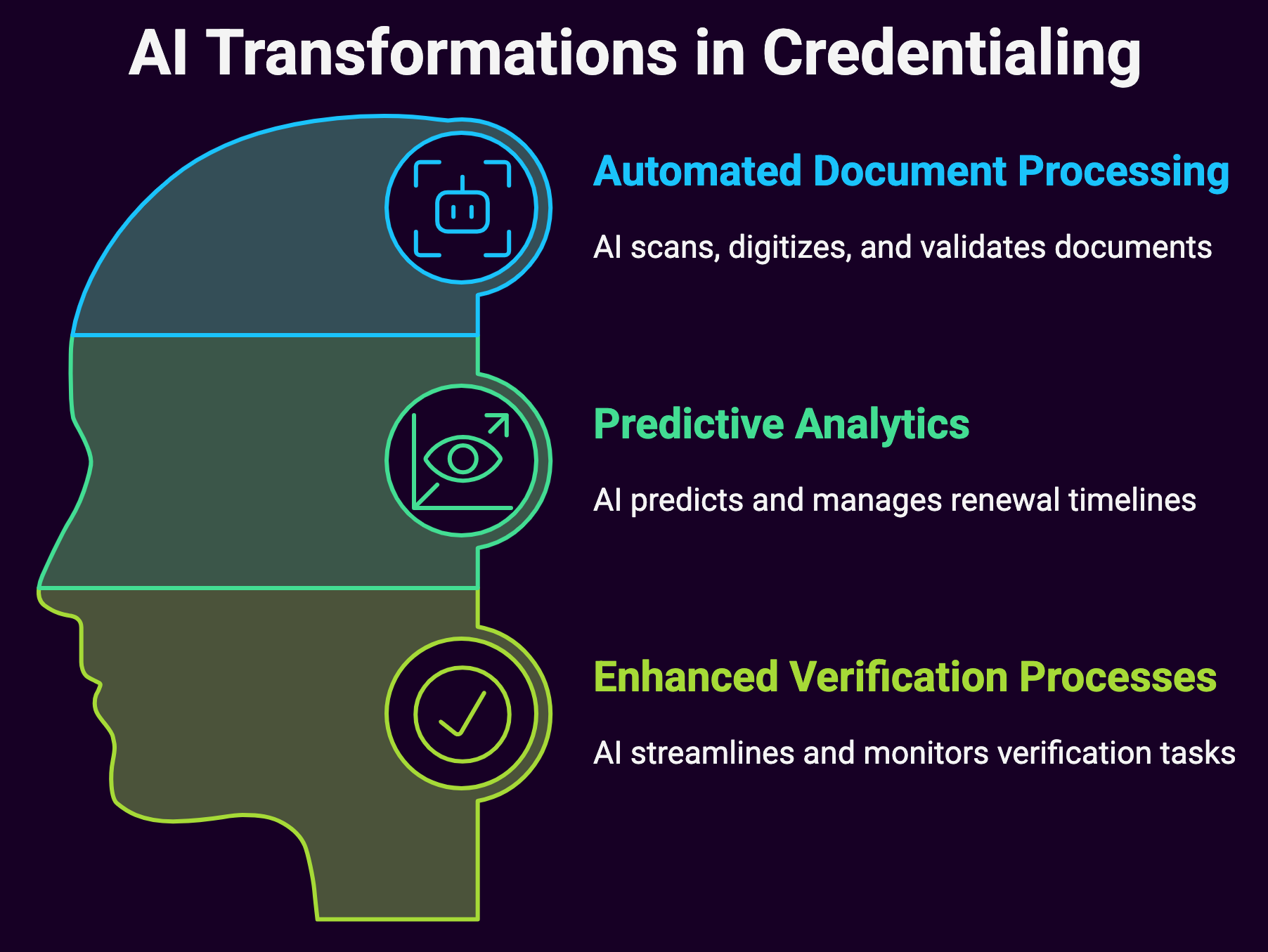
Automated Document Processing
Remember those towering stacks of paperwork? AI-powered Optical Character Recognition (OCR) technology can now scan and digitize documents in seconds, extracting relevant information automatically. But it goes beyond simple data extraction.
Modern AI systems can:
- Validate information accuracy in real-time
- Flag discrepancies or missing information
- Cross-reference data across multiple sources
- Update provider databases automatically
Predictive Analytics for Renewal Management
One of the most impressive applications of AI in credentialing is its ability to predict and manage renewal timelines.
These systems can:
- Generate automated alerts for upcoming expirations
- Identify patterns in processing times
- Recommend optimal submission windows
- Prioritize urgent renewals based on historical data
Enhanced Verification Processes
Primary source verification, once a time-consuming manual process, has been streamlined through AI.
Modern systems can:
- Automatically verify licenses across state databases
- Check sanctions and exclusion lists in real-time
- Monitor ongoing compliance requirements
- Alert staff to potential red flags or concerns
The Numbers Don’t Lie
Let’s talk about impact.
Healthcare organizations implementing AI-driven credentialing solutions report:
- 60% reduction in processing time
- 80% decrease in manual data entry errors
- 50% lower administrative costs
- 90% improvement in provider satisfaction
These aren’t just statistics; they represent real improvements in healthcare delivery and access to care.
Real-World Applications
Consider the experience of Metropolitan Health System, which implemented an AI-powered credentialing solution in 2023. “The transformation was remarkable,” notes their Chief Medical Officer, Dr. James Chen. “What used to take our team months now takes weeks, sometimes even days. But more importantly, the accuracy of our credentialing process has improved significantly.”
Their success story isn’t unique.
Here’s what healthcare organizations are achieving with AI-driven credentialing:
Continuous Monitoring
Modern AI systems don’t just assist with initial credentialing; they provide ongoing monitoring of:
- License status changes
- Disciplinary actions
- Malpractice claims
- Board certification updates
Intelligent Workflow Management
AI algorithms can:
- Prioritize applications based on urgency and complexity
- Route tasks to appropriate team members
- Identify bottlenecks in the process
- Suggest workflow optimizations
Enhanced Compliance
With regulatory requirements constantly evolving, AI helps organizations:
- Stay current with changing regulations
- Ensure consistent policy application
- Maintain detailed audit trails
- Generate compliance reports automatically
Challenges and Considerations
Of course, it’s not all smooth sailing.
The integration of AI into medical credentialing comes with its own set of challenges:
Data Security and Privacy
With sensitive provider information at stake, organizations must ensure:
- Robust encryption protocols
- Secure data storage and transmission
- Compliance with HIPAA and other regulations
- Regular security audits and updates
Initial Implementation Hurdles
Organizations often face:
- Resistance to change from staff
- Integration with existing systems
- Training requirements
- Initial cost considerations
Quality Control
While AI can greatly improve accuracy, human oversight remains crucial for:
- Complex decision-making
- Unusual cases or exceptions
- Final verification and approval
- Relationship management
Looking to the Future
The role of AI in medical credentialing continues to evolve.
Emerging trends include:
Blockchain Integration
Blockchain technology combined with AI could:
- Create immutable credentialing records
- Enable instant verification
- Reduce fraud risks
- Streamline cross-organizational sharing
Advanced Machine Learning
Next-generation AI systems will:
- Learn from historical decisions
- Provide more accurate predictions
- Offer sophisticated risk assessments
- Automate complex decision-making
Expanded Integration
Future systems will likely feature:
- Seamless integration with EMR systems
- Real-time updates across platforms
- Enhanced interoperability
- Mobile-first solutions
Best Practices for Implementation
For organizations considering AI-powered credentialing solutions, consider these key steps:
Assessment and Planning
- Evaluate current processes
- Identify pain points
- Set clear objectives
- Develop implementation timeline
Vendor Selection
- Research available solutions
- Check references
- Verify security protocols
- Ensure scalability
Staff Training
- Provide comprehensive training
- Address concerns proactively
- Establish support systems
- Monitor adoption rates
Continuous Improvement
- Gather feedback regularly
- Monitor key metrics
- Adjust processes as needed
- Stay current with updates
The Human Element
While AI is revolutionizing medical credentialing, it’s important to remember that technology isn’t replacing humans, it’s empowering them. As Micah Schultz notes, “AI handles the routine tasks that used to consume my day. Now I can focus on complex cases, building relationships with providers, and improving our processes.”
Summary: AI in Credentialing
![]() The integration of AI into credentialing represents more than just technological advancement; it’s a fundamental shift in how healthcare organizations approach this critical function. Automating routine tasks, improving accuracy, and enabling proactive management are the key. AI is helping organizations create more efficient, effective credentialing processes.
The integration of AI into credentialing represents more than just technological advancement; it’s a fundamental shift in how healthcare organizations approach this critical function. Automating routine tasks, improving accuracy, and enabling proactive management are the key. AI is helping organizations create more efficient, effective credentialing processes.
It’s easy to see, AI will continue to play an increasingly important role in credentialing. Organizations that embrace these technologies while maintaining appropriate human oversight will be best positioned to thrive. The goal isn’t to eliminate the human element from credentialing, but to enhance it. Leveraging AI’s capabilities allows healthcare organizations to create more efficient, accurate, and responsive credentialing processes that benefit everyone, administrators, providers, and ultimately, patients.
Ensuring qualified healthcare providers can deliver care to those who need it, as quickly and efficiently as possible. This is what ultimately matters!
Contact us to assist with your credentialing needs and/or challenges.

