Medical billing automation is probably not going to win any awards for being a riveting conversation topic. It’s one of those mundane but necessary evils that come with running a healthcare organization. I get it – discussing billing processes and paperwork isn’t exactly a thrilling way to spend your time. But hear me out, because this is one of those areas where making some behind-the-scenes improvements can have a huge positive impact on your operations. A little proactive optimization of billing workflows can go a remarkably long way in boosting efficiency, cutting costs, and ensuring you get paid properly for services rendered. So while it may not set your heart racing with excitement, it’s worth a few minutes of your attention.
Dealing With Manual Medical Billing Woes
If you work in healthcare administration or have any experience with medical billing, you know just how tedious and error-prone the manual billing process can be. It’s a lot of data entry, cross-checking information across different systems and databases, following complex rules and guidelines. One little slip-up and you could be looking at denied claims, unhappy patients, and a whole lot of headaches.
Even the most meticulous billing specialists can make mistakes when overwhelmed with monotonous, high-volume tasks. Typos happen. Numbers get transposed. Little details get overlooked. It’s just human nature, as much as we’d like to be perfect automatons.
These kinds of errors in medical billing don’t just create more work in having to revisit and resubmit claims.
They can lead to some serious consequences like:
- Delayed payments and cash flow issues for healthcare providers
- Compliance violations and potential penalties
- Lower patient satisfaction due to incorrect billing
- Hours of employee time spent on remediation instead of higher-value work
So it’s clear that finding ways to minimize billing errors should be a top priority, right? But how can we realistically reduce these types of avoidable mistakes without hiring a small army of billing specialists? That’s where robotic process automation (RPA) comes into play.
What is RPA? Your New Digital Workforce
Think of RPA as a way to create a virtual, software-based workforce to handle those repetitive, rules-based tasks that have been bogging down your human employees. At its core, RPA uses coded software “robots” to mimic the actions that billing specialists and other workers perform on a computer – everything from data entry and calculations to automated decisions and routing work between systems.
These software robots can work tirelessly around the clock without getting fatigued or making careless mistakes. They diligently follow every rule and workflow to the letter, never deviating unless that’s what their coding instructs. And they don’t get bored or distracted by the monotonous nature of highly transactional processes.
Now, I can already hear some of you going “But we already have automation and scripting tools that handle certain parts of our billing process.” And you’d be absolutely right! RPA is not meant to fully replace those existing automation capabilities, but to work alongside them in an integrated way.
The key difference is that RPA is a more flexible and versatile layer of automation. It operates at the user interface level, just like a human would. So it can be deployed to streamline processes and tasks across different applications and systems, even in environments with legacy IT systems that can’t be seamlessly integrated or modified.
This is hugely valuable when you have medical billing scenarios that involve swiveling between different practice management software, electronic health records (EHR) systems, payment portals, and other data sources. RPA can act as a hub coordinating all of those systems.
Taking Medical Billing to the RPA Bot
So how exactly can you put RPA to work in minimizing errors for those manual medical billing headaches?
Let’s go through some of the prime use cases:
Intake and Data Entry
A huge portion of the medical billing process is just getting information from different sources into the right billing system accurately. Whether it’s entering patient demographics, scanning documents and attaching them properly, or collecting insurance details – there are so many opportunities for small data entry goofs.
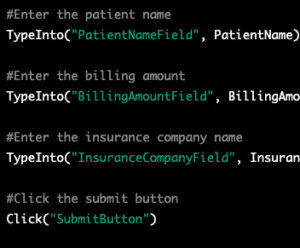
RPA bots can be trained to systematically collect and validate data from patient records, image files, EDI transmissions and other sources. They can cross-reference information between multiple systems to ensure consistency. Rules can be encoded to automatically flag any missing or incorrect data that needs review.
Once that data has been verified, the bots can take over the rote process of punching everything into the billing software precisely as expected, without any unforced errors. No more mistyped numbers or transposed codes.
Code Checking and Auditing
Applying the right medical codes is obviously critical for billing accuracy and ensuring claims are approved properly. But keeping up with all the updated code sets and regulations is an ongoing challenge. Billing specialists constantly have to cross-check their coding against changing guidelines and payer-specific criteria.
RPA bots can be programmed with the latest coding rules and automate those auditing steps. They can comb through billing entries and flag any codes that may be incorrect or any cases where additional documentation is required for a particular code. For complicated scenarios, bots may be able to automatically determine the right codes by processing structured data inputs based on pre-defined decision rules.
Again, this is something humans can certainly do, but are much more prone to making mistakes, unlike RPA bots. By automating those code checks and validations, you eliminate a major vector for billing errors.
Prioritization and Workload Balancing
At high-volume billing operations, it’s critical to prioritize the most urgent claims while juggling workloads across billing staff. Managers have to assess queues and utilization continuously to determine what work to allocate to who. This process becomes even trickier when you factor in employee vacations, sick days, and turnovers.
RPA can be immensely useful in automating those prioritization and workload balancing processes based on pre-defined business rules and objectives. Bots can be scheduled to routinely scan billing queues and distribute work appropriately across available human and bot resources. They can automatically prioritize billing tasks based on parameters like client priority, aging of claims, and expected reimbursement amount.
Monitoring and Exception Handling
Of course, even with RPA automating a lot of the manual tasks, there will always be some percentage of billing entries and claims that need higher-level exception handling. Maybe it’s an edge case scenario not covered by automation rules. Or maybe there are additional documentation requirements that billing specialists need to handle.
In those cases, RPA can still play a pivotal role in monitoring automated processes and triggering steps for human intervention when needed. Bots can be trained to identify exceptions based on certain data conditions and automatically route those cases to billing specialists for further review. Dashboards and escalation workflows can be set up so those exceptions get addressed in a timely, organized manner.
The bots can also handle follow-up steps after human review has been completed. For example, submitting cleared claims directly to payers, updating systems with notes and comments from the specialist’s review, and logging audit trails.
Key Enablers of Successful RPA in Medical Billing
I don’t want to make it sound like implementing RPA solutions for billing processes is as easy as downloading some software and clicking a few buttons.
There are some key elements that need to be in place:
Clear Process Documentation and Rules
RPA is really good at automating processes, but only if those processes and workflows are clearly documented and defined. If there isn’t a logical, consistent set of rules codified for how medical billing works at an organization – across all the different types of services, specialties, data handoffs, and systems involved – then RPA becomes much harder.
So investing time and effort into mapping out those end-to-end processes exhaustively is crucial for RPA success. It’s also an opportunity to find ways to streamline and optimize processes before automating them.
Data Consolidation and Cleanup
RPA bots need access to accurate, high-quality data from consolidated sources in order to function effectively. Any underlying data quality issues like duplicates, inconsistencies, and siloed datasets have to be addressed. Oftentimes, data integration and cleansing work may be required ahead of RPA deployment.
There’s also a need for data process experts who intimately understand the structure, fields, and flows of billing data across systems. This type of SME guidance is necessary for properly scoping and defining automation workflows that RPA bots will handle.
Change Management and Governance
Once medical billing processes are automated through RPA, there needs to be governance around how changes get implemented and managed. Finance and operations teams should define procedures for vetting any alterations to automated processes, testing them in dev environments, and versioning bot deployments.
Having a centralized RPA Center of Excellence (COE) to oversee this change management is highly recommended. The COE can also provide training and support resources for billing staff who will be working alongside digital bot workers.
A measured rollout plan that implements RPA use cases in phases can help facilitate user adoption too. Just introducing dozens of bots to replace entire processes all at once will likely be disruptive.
Strategic RPA Implementation Approach
Speaking of rollout plans, it’s important to be deliberate and strategic about how RPA is introduced to your billing operations, rather than taking a blind “automate everything” approach. Take stock of where your biggest billing challenges, risks, and cost centers are currently. Then prioritize implementing RPA use cases that tackle those critical pain points first.
Start with high-volume, repetitive billing tasks that are prime candidates for automation. Or target areas that have been major sources of errors, delays, and compliance issues. Quick wins that provide immediate ROI and improved efficiency will help build momentum for further RPA adoption.
At the same time, don’t just hyper-focus on automating tedious tasks to reduce headcounts. Look for opportunities where RPA can help upskill billing staff by taking over manual drudge work so they can focus on higher-value activities. Things like performing root cause analysis on billing errors, managing audits and appeals, or optimizing processes.
Integrating intelligent capabilities like machine learning and natural language processing alongside RPA can elevate what’s possible too. You could have bots automatically read and comprehend billing documentation, or predict billing code requirements based on historical data.
The Road to Automation
Implementing RPA for medical billing processes won’t happen overnight, but the long-term benefits of reducing errors and streamlining operations make it well worth the effort. By establishing the right governance, changing management practices, and strategic approach, providers can ultimately realize substantially more accurate and cost-efficient revenue cycle performance.
Even with the rise of artificial intelligence and machine learning, good old-fashioned process automation will remain crucial in healthcare. Billing is one of those areas ripe for applying RPA to drive out costly mistakes and free up human employees to focus on higher-value work. It’s the ultimate “better together” story of human and digital labor collaborating.
So don’t think of billing bots as job-stealing enemies, but as dutiful assistants helping ensure you get paid accurately and on time for the vital healthcare services your organization provides. Less time wrestling with billing errors frees you up to spend more quality time with patients. And really, isn’t that what healthcare is all about?

