Provider credentialing isn’t exactly the most glamorous part of healthcare administration. If you’re responsible for ensuring your organization meets credentialing standards, you know just how critical this process is to your operations, reputation, and bottom line. When it comes to credentialing standards, one name stands above the rest: NCQA.
 The National Committee for Quality Assurance (NCQA) has established itself as the gold standard for credentialing in healthcare. Their guidelines don’t just represent best practices. They’ve become essential requirements for organizations seeking to demonstrate quality, maintain accreditation, and secure contracts with payers.
The National Committee for Quality Assurance (NCQA) has established itself as the gold standard for credentialing in healthcare. Their guidelines don’t just represent best practices. They’ve become essential requirements for organizations seeking to demonstrate quality, maintain accreditation, and secure contracts with payers.
Navigating NCQA standards can feel like trying to read a map in a foreign language. The requirements are detailed, the documentation is extensive, and the stakes are high. One misstep can lead to delayed accreditation, compliance issues, or worse.
Understanding NCQA
Before analyzing the specifics of NCQA’s credentialing standards, it’s worth understanding what this organization is and why their guidelines carry so much weight in the healthcare industry.
What Is NCQA?
The National Committee for Quality Assurance is an independent, nonprofit organization founded in 1990 with a mission to improve healthcare quality. Unlike regulatory bodies that establish minimum requirements, NCQA sets aspirational standards designed to drive continuous quality improvement.
NCQA is best known for its Health Plan Accreditation program, but its influence extends to many aspects of healthcare quality, including provider credentialing. Organizations that achieve NCQA accreditation demonstrate their commitment to quality care and operational excellence.
Why NCQA Standards Matter
You might be wondering: “With so many regulatory requirements in healthcare, why should I care specifically about NCQA standards?”
Here are several compelling reasons:
- Payer requirements: Many health plans require their network providers to follow NCQA credentialing standards. Meeting these standards can be essential for securing and maintaining contracts.
- Risk management: Thorough credentialing following NCQA guidelines helps protect your organization from liability associated with provider-related incidents.
- Quality improvement: NCQA standards aren’t just about checking boxes—they’re designed to enhance the quality of your provider network and, by extension, patient care.
- Competitive advantage: In an increasingly competitive healthcare landscape, NCQA accreditation can differentiate your organization and attract both patients and providers.
- Operational efficiency: While implementing NCQA standards requires up-front investment, they ultimately promote standardized, efficient credentialing processes.
The Core NCQA Credentialing Standards
NCQA’s credentialing standards are organized into categories that cover every aspect of the credentialing process. Let’s walk through these core standards and what they mean for your organization.
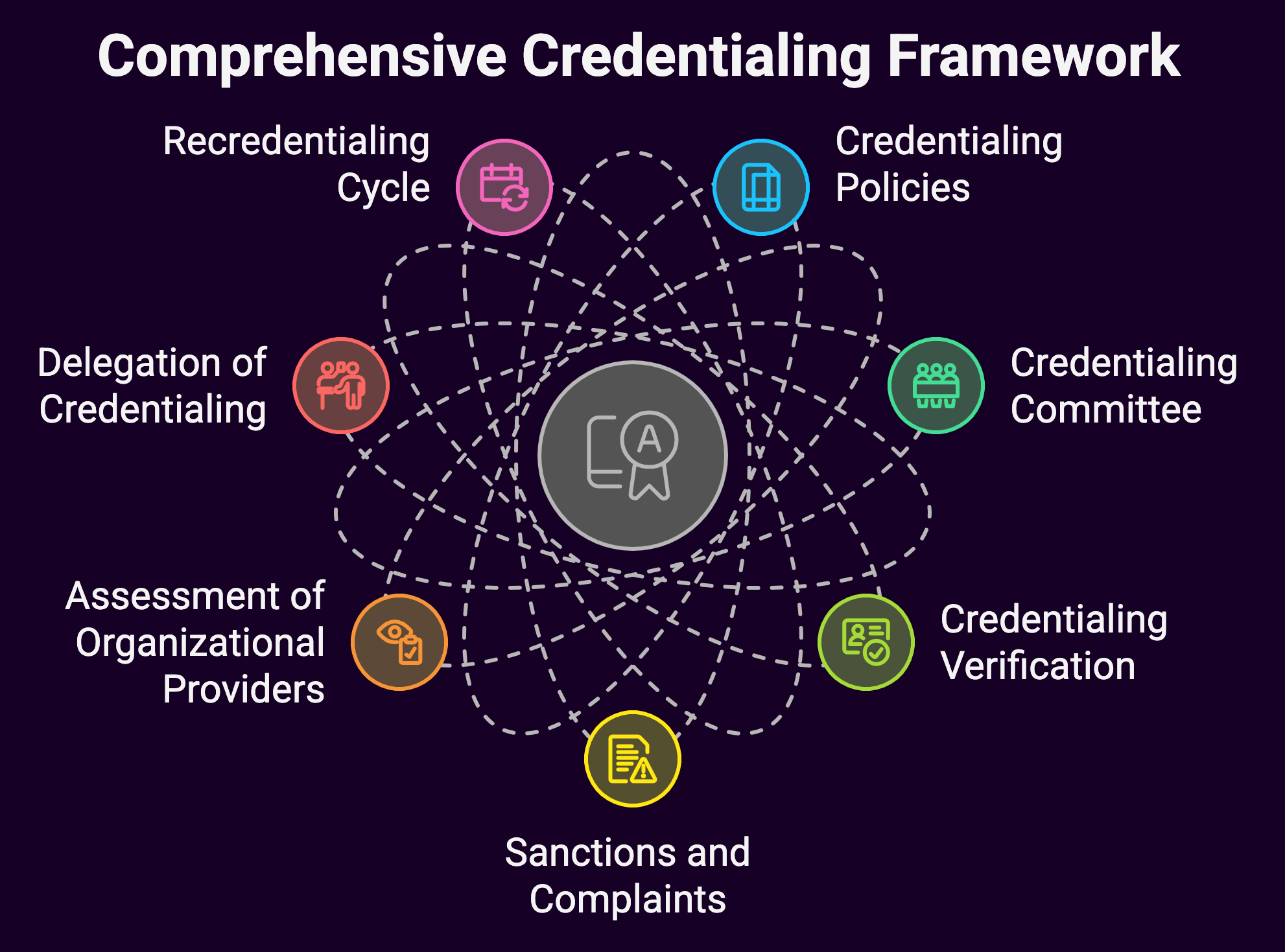
CR 1: Credentialing Policies
The foundation of NCQA-compliant credentialing is a robust set of policies that clearly define your processes.
These policies must address:
- The types of practitioners subject to credentialing and recredentialing
- The information collected and verified during the credentialing process
- How credentialing decisions are made
- Procedures for notifying practitioners of decisions
- Timeframes for processing applications
- Policies for ongoing monitoring between recredentialing cycles
Key requirement: Your policies must be approved by a designated committee, reviewed annually, and updated as needed.
Common pitfall: Many organizations have policies that don’t reflect their actual practices. Your documented policies should match your real-world processes, and vice versa.
CR 2: Credentialing Committee
NCQA standards require a formal decision-making body—typically a credentialing committee—with responsibility for credentialing decisions.
Requirements for this committee include:
- A defined membership structure with appropriate clinical representation
- Regular meetings (at least quarterly) with documented minutes
- Review of credentials for practitioners who don’t meet established criteria
- Clear decision-making processes
Key requirement: The committee must include representation from various specialties to ensure appropriate peer review.
Common pitfall: Insufficient documentation of committee deliberations and rationale for decisions, particularly for cases that don’t meet standard criteria.
CR 3: Credentialing Verification
This standard addresses the heart of credentialing: verification of provider qualifications.
NCQA specifies:
- Which credentials must be verified
- Acceptable verification sources (primary vs. secondary)
- Timeframes for verification (typically 180 days before credentialing decision)
- Documentation requirements for verification activities
Credentials that require primary source verification include:
- Licensure: Current, valid license to practice
- DEA/CDS certification: For providers who prescribe controlled substances
- Education and training: Including medical school, residency, and fellowship
- Board certification: If claimed by the provider
- Work history: Minimum of five years with explanation of gaps over six months
- Malpractice history: Claims history and verification of current malpractice insurance
- Sanctions and exclusions: Checks against the OIG, SAM, and other databases
Key requirement: Organizations must document the method, source, and date of each verification.
Common pitfall: Relying on expired verifications or failing to document the verification process adequately.
CR 4: Sanctions and Complaints
NCQA requires ongoing monitoring of sanctions, complaints, and adverse events between formal recredentialing cycles.
This standard covers:
- Monthly checks of state licensing boards and federal sanction databases
- Processes for reviewing and acting on complaints
- Procedures for addressing adverse events and quality concerns
Key requirement: Organizations must demonstrate their process for receiving and reviewing Medicare and Medicaid sanctions and limitations on licensure.
Common pitfall: Failing to establish a systematic, ongoing monitoring process or not documenting actions taken in response to identified issues.
CR 5: Assessment of Organizational Providers
This standard applies to facilities rather than individual practitioners.
Organizations must:
- Confirm that facilities have appropriate licensure and accreditation
- Verify malpractice insurance coverage
- Review Medicare/Medicaid sanctions
- Reassess facilities at least every three years
Key requirement: Organizations must have a process for assessing non-accredited facilities against their own standards.
Common pitfall: Applying individual practitioner standards to facilities instead of facility-specific criteria.
CR 6: Delegation of Credentialing
If your organization delegates any part of the credentialing process to another entity (such as a CVO or medical group), this standard applies.
Requirements include:
- Written delegation agreements that specify responsibilities
- Annual evaluation of the delegate’s performance
- Regular reporting from the delegate
- Procedures for revoking delegation if standards aren’t met
Key requirement: Your organization remains responsible for ensuring delegates meet NCQA standards, even if credentialing activities are outsourced.
Common pitfall: Insufficient oversight of delegated activities and inadequate documentation of delegate performance.
CR 7: Recredentialing Cycle
Providers must be recredentialed at least every three years.
Recredentialing includes:
- Verification of current licensure and other credentials
- Review of performance indicators
- Assessment of member complaints and satisfaction data
- Evaluation of utilization patterns and quality metrics
Key requirement: Organizations must have systems to track recredentialing due dates and ensure timely completion.
Common pitfall: Missing recredentialing deadlines due to inadequate tracking systems or process delays.
Practical Implementation: Turning Standards into Action
Understanding NCQA standards is one thing; implementing them effectively is another. It’s important to take practical approaches to meeting these requirements in your organization.
Building an NCQA-Compliant Credentialing Program
If you’re establishing a new credentialing program or revamping an existing one, consider these steps:
- Gap analysis: Compare your current policies and processes to NCQA standards to identify areas needing improvement.
- Policy development: Create comprehensive policies that address all NCQA requirements while reflecting your organization’s specific needs and culture.
- Committee structure: Establish a credentialing committee with appropriate representation and clearly defined authority.
- Process mapping: Document your credentialing workflow from application receipt to decision, ensuring each step aligns with NCQA requirements.
- Documentation systems: Implement robust documentation practices that capture all required verification activities and decision-making processes.
- Training program: Ensure staff understand NCQA requirements and your organization’s specific procedures.
- Monitoring mechanisms: Develop systems for ongoing monitoring of sanctions and performance issues between recredentialing cycles.
Technology Solutions for NCQA Compliance
While NCQA standards don’t require specific technology, the right systems can significantly facilitate compliance:
- Credentialing software: Modern platforms can automate verification processes, track expiration dates, and generate alerts for required actions.
- Document management systems: Secure, searchable repositories for credentialing documentation support efficient verification and audit preparation.
- Provider portals: Self-service portals allow providers to submit and update their information, reducing administrative burden and improving accuracy.
- Reporting tools: Advanced analytics can help identify trends, track performance metrics, and generate required reports.
- Integration capabilities: Systems that connect with primary verification sources can streamline the verification process and reduce manual effort.
When evaluating technology solutions, look for:
- NCQA-specific features: Some platforms are designed specifically to support NCQA compliance.
- Customization options: Your system should adapt to your specific policies and workflows.
- Audit support: Look for robust reporting features that facilitate NCQA surveys and internal audits.
- Scalability: Choose a solution that can grow with your organization.
- User-friendliness: Complex systems that staff struggle to use correctly can create compliance risks.
Preparing for an NCQA Survey
If your organization is pursuing NCQA accreditation, preparation is key to success.
Here’s how to get ready:
12-18 months before survey:
- Conduct a thorough gap analysis against current NCQA standards
- Develop an implementation plan to address identified gaps
- Ensure policies and procedures are updated and approved
- Begin collecting and organizing documentation
6-12 months before survey:
- Conduct internal audits of credentialing files
- Review committee minutes for completeness
- Address any identified deficiencies
- Ensure all delegates meet NCQA requirements
3-6 months before survey:
- Conduct a mock survey
- Fine-tune processes based on mock survey results
- Ensure all staff are trained on NCQA requirements
- Organize documentation according to NCQA standards
1-3 months before survey:
- Finalize all documentation
- Conduct final file audits
- Prepare staff for interviews
- Review most recent NCQA updates and clarifications
Common Challenges and Solutions
Even organizations committed to NCQA compliance often encounter obstacles.
Here are some common challenges and strategies to overcome them:
Challenge 1: Keeping Up with Standard Changes
NCQA regularly updates its standards to reflect evolving best practices and industry changes. Staying current can be challenging.
Solutions:
- Assign staff responsibility for monitoring NCQA updates
- Subscribe to NCQA newsletters and alerts
- Participate in NCQA educational programs
- Join industry groups focused on credentialing
- Consider engaging consultants for major standard revisions
Challenge 2: Primary Source Verification Difficulties
Obtaining timely responses from primary sources can delay the credentialing process and create compliance risks.
Solutions:
- Develop relationships with key verification sources
- Implement tracking systems for outstanding verifications
- Establish clear escalation procedures for delayed responses
- Consider NCQA-certified Credentials Verification Organizations (CVOs) for challenging verifications
- Document all verification attempts thoroughly
Challenge 3: Provider Engagement
Collecting complete, accurate information from providers is essential but often difficult.
Solutions:
- Create user-friendly application processes
- Provide clear instructions and expectations
- Implement automated reminders for missing information
- Develop positive relationships with provider office staff
- Consider incentives for timely, complete submissions
Challenge 4: Delegation Management
Organizations that delegate credentialing functions often struggle with oversight and documentation.
Solutions:
- Develop comprehensive delegation agreements
- Implement regular reporting requirements
- Conduct annual evaluations using standardized tools
- Maintain open communication with delegates
- Consider technology solutions that facilitate oversight
Challenge 5: Resource Constraints
Many organizations face staffing and budget limitations that make comprehensive compliance challenging.
Solutions:
- Prioritize high-risk areas for immediate attention
- Consider outsourcing specific functions
- Implement technology to increase efficiency
- Develop phased implementation plans
- Cross-train staff to provide coverage and flexibility
Beyond Basic Compliance: Excellence in Provider Credentialing
While meeting NCQA standards is essential, truly exceptional organizations go beyond minimum requirements to create credentialing programs that enhance quality and efficiency.
Integrating Credentialing with Quality Improvement
Forward-thinking organizations connect credentialing with broader quality initiatives by:
- Incorporating meaningful quality metrics into recredentialing decisions
- Aligning credentialing criteria with organizational quality goals
- Using credentialing data to identify opportunities for improvement
- Involving the credentialing committee in quality improvement activities
- Providing credentialing data to clinical leadership for targeted interventions
Creating a Positive Provider Experience
The credentialing process significantly impacts provider satisfaction and can influence recruitment and retention.
Leading organizations:
- Streamline applications to collect only necessary information
- Provide transparent timelines and status updates
- Offer support resources for providers navigating the process
- Gather and act on provider feedback about the credentialing experience
- Use technology to reduce administrative burden
Developing Staff Excellence
The effectiveness of your credentialing program ultimately depends on your team.
Excellence requires:
- Comprehensive training on NCQA standards and organizational policies
- Clear performance expectations and accountability
- Regular education on industry developments and best practices
- Recognition and reward for quality and compliance
- Development opportunities that enhance expertise and engagement
The Future of NCQA Credentialing Standards
As healthcare continues to evolve, NCQA standards will inevitably change to reflect new priorities and best practices.
Here are some trends to watch:
Increased Focus on Telehealth
The rapid expansion of telehealth services is likely to influence credentialing standards, with greater attention to:
- Interstate licensure verification
- Telehealth-specific competencies
- Remote practice monitoring
- Technology proficiency assessment
Enhanced Provider Performance Evaluation
Future standards may place greater emphasis on:
- Patient-reported outcome measures
- Social determinants of health considerations
- Team-based care effectiveness
- Specific population health metrics
Technology Integration
As technology continues to transform credentialing, NCQA is likely to address:
- Blockchain and distributed ledger technologies for credential verification
- Artificial intelligence applications in credentialing
- Virtual primary source verification
- Digital provider passports
Alignment with Value-Based Care
As healthcare continues to shift toward value-based models, credentialing standards may evolve to incorporate:
- Cost-effectiveness measures
- Value-based contract performance
- Population health management capabilities
- Preventive care effectiveness
Summary: The Strategic Value of NCQA Compliance
NCQA credentialing standards represent far more than a compliance requirement. They provide a framework for building a high-quality provider network that delivers exceptional care. Organizations that embrace these standards position themselves for success in an increasingly competitive and quality-focused healthcare environment.
Effective implementation requires commitment from leadership, dedicated resources, and a culture that values quality and continuous improvement. The rewards, which include enhanced patient safety, improved provider relations, operational efficiency, and competitive advantage, make the investment worthwhile.

