In credentialing for Advanced Practice Providers (APPs), you’ve probably noticed it’s not quite the same as physician credentialing. Whether you’re an APP yourself, a credentialing specialist, or a healthcare administrator, understanding these unique requirements is crucial for smooth sailing through the credentialing process. Let’s break down everything you need to know about APP credentialing, from the basics to the granular details.
Understanding APP Categories and Scope
Let’s garner some clarity on who we’re talking about when we say “Advanced Practice Providers.”
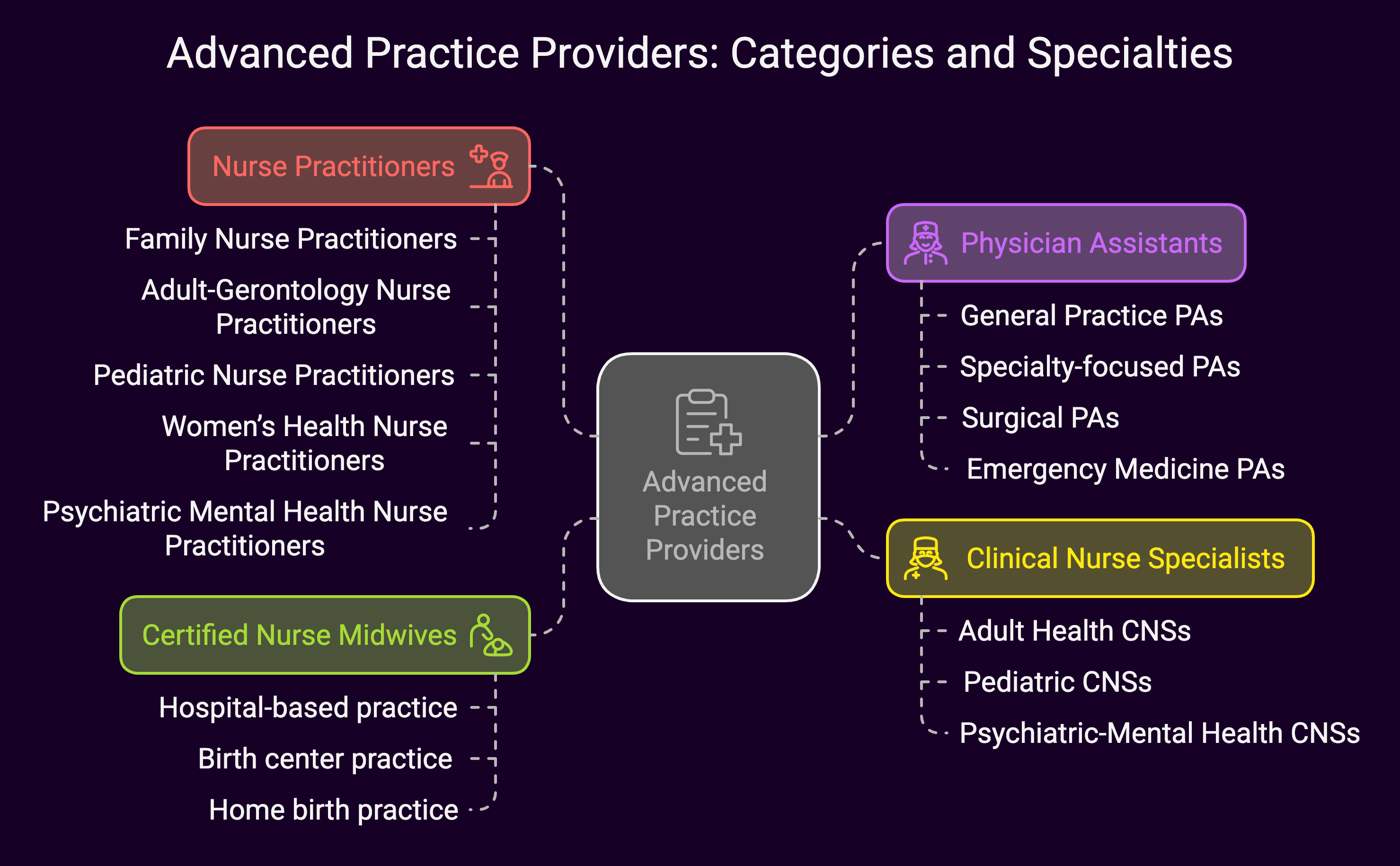
This umbrella term includes:
 Nurse Practitioners (NPs)
Nurse Practitioners (NPs)
- Family Nurse Practitioners (FNPs)
- Adult-Gerontology Nurse Practitioners (AGNPs)
- Pediatric Nurse Practitioners (PNPs)
- Women’s Health Nurse Practitioners (WHNPs)
- Psychiatric Mental Health Nurse Practitioners (PMHNPs)
Physician Assistants (PAs)
- General Practice PAs
- Specialty-focused PAs
- Surgical PAs
- Emergency Medicine PAs
Clinical Nurse Specialists (CNSs)
- Adult Health CNSs
- Pediatric CNSs
- Psychiatric-Mental Health CNSs
Certified Nurse Midwives (CNMs)
- Hospital-based practice
- Birth center practice
- Home birth practice
Core Credentialing Requirements
Let’s jump into the essential requirements that apply to all APPs, regardless of specialty or state:
Educational Verification
- Graduate degree (Master’s or Doctoral level)
- Specialized training programs
- Clinical rotations documentation
- Continuing education requirements
Licensure and Certification
- State licensure requirements
- National certification through appropriate boards
- DEA registration (if applicable)
- State-specific controlled substance registrations
Clinical Experience
- Documentation of supervised practice hours
- Specialty-specific experience
- Procedure logs (if applicable)
- Clinical competency evaluations
Background Screening
- Criminal background checks
- OIG/GSA exclusion lists
- State-specific background requirements
- Professional reference checks
Collaborative Agreement Considerations
One of the biggest differences in APP credentialing is the collaborative agreement requirement.
Let’s break this down:
Required Elements
- Scope of practice definition
- Consultation requirements
- Prescription authority limits
- Chart review protocols
- Coverage arrangements
State Variations
- Full practice authority states
- Reduced practice authority states
- Restricted practice authority states
Documentation Requirements
- Written agreement format
- Filing requirements with state boards
- Regular review and updates
- Emergency backup arrangements
State-Specific Requirements
Just like with physician credentialing, state requirements can vary significantly.
Here’s what you need to know:
Full Practice Authority States
- No physician supervision required
- Independent prescribing authority
- Direct patient care responsibility
- Independent practice locations
Reduced Practice Authority States
- Collaborative agreement required
- Partial prescribing independence
- Regular physician consultation
- Practice location restrictions
Restricted Practice Authority States
- Direct physician supervision required
- Limited prescribing authority
- Mandatory chart reviews
- Strict practice location requirements
Privileging Process
The privileging process for APPs has its own unique considerations:
Initial Privileging
- Core privilege determination
- Specialty-specific privileges
- Procedure-specific privileges
- Educational requirements verification
Ongoing Monitoring
- Quality metrics tracking
- Patient satisfaction data
- Peer review process
- Outcome measurements
Expansion of Privileges
- Additional training documentation
- Competency verification
- Procedure logs
- Supervisor recommendations
Insurance and Payer Enrollment
Getting APPs properly enrolled with insurance companies requires attention to detail:
Medicare Enrollment
- Individual NPI requirements
- Medicare billing rules
- Incident to” billing considerations
- Direct billing requirements
Private Payer Enrollment
- Payer-specific requirements
- Credentials verification organization (CVO) process
- Reimbursement variations
- Contract negotiations
Malpractice Insurance
- Coverage requirements
- Limits determination
- Tail coverage considerations
- Claims history documentation
Common Challenges and Solutions
Let’s address some frequent hurdles in APP credentialing:
Challenge 1: Varying State Requirements
Solution:
- Create state-specific checklists
- Maintain updated requirement databases
- Use tracking software
- Regular requirement reviews
Challenge 2: Collaborative Agreement Changes
Solution:
- Develop standardized agreement templates
- Create change notification systems
- Maintain backup collaborator lists
- Regular agreement reviews
Challenge 3: Privilege Documentation
Solution:
- Implement procedure logging systems
- Regular competency assessments
- Clear documentation protocols
- Standardized evaluation forms
Best Practices and Tips
Here’s what successful organizations do to streamline APP credentialing:
Documentation Management
- Create digital folders for each provider
- Implement automatic renewal reminders
- Use standardized forms
- Maintain backup copies
Process Optimization
- Develop clear workflows
- Create timeline expectations
- Use automation where possible
- Regular process reviews
Communication Strategies
- Regular updates to stakeholders
- Clear notification systems
- Documentation of conversations
- Standardized communication templates
Future Trends and Changes
The APP credentialing landscape is constantly evolving.
Here’s what to watch for:
Regulatory Changes
- Expanding scope of practice
- Changing supervision requirements
- New privileging considerations
- Updated payer requirements
Technology Integration
- Digital credentialing platforms
- Blockchain verification systems
- Automated tracking systems
- Electronic document management
Practice Evolution
- Telemedicine considerations
- Multi-state practice requirements
- New specialty development
- Changed practice models
Best Practices for Success
To wrap things up, here are some key takeaways for successful APP credentialing:
1. Stay Organized
- Maintain detailed checklists
- Keep current documentation
- Track expiration dates
- Document all communications
2. Build Strong Relationships
- Regular provider communication
- Clear expectations setting
- Open feedback channels
- Collaborative problem-solving
3. Keep Current
- Regular requirement updates
- Continuing education tracking
- Professional development monitoring
- Policy/procedure reviews
4. Use Available Resources
- Professional organizations
- Credentialing software
- State board resources
- Legal consultation when needed
Summary: Advanced Practice Providers Credentialing
Credentialing for Advanced Practice Providers might seem complex, but with the right approach and understanding, it can be managed effectively. With requirements dynamically evolving, particularly as APPs gain more practice authority across states, staying informed about changes and maintaining organized systems will help ensure successful credentialing outcomes.
The key to success lies in understanding the unique aspects of APP credentialing while maintaining flexibility to adapt to changing requirements. It doesn’t matter if you’re managing credentialing for a single APP or an entire team, following these guidelines will help create a smooth and efficient process.


 Nurse Practitioners (NPs)
Nurse Practitioners (NPs)