Healthcare providers seeking to practice across state lines face a complex web of regulatory requirements, administrative hurdles, and evolving legal frameworks. Multi-state licensing has become increasingly important in an era of telehealth expansion, provider shortages, and healthcare delivery models that transcend traditional geographic boundaries. The undermentioned content is an examination of the current landscape, challenges, and emerging solutions in multi-state provider credentialing.
The Foundation of State-Based Licensing
The United States maintains a decentralized approach to healthcare provider licensing, with each state exercising independent authority through state medical boards and regulatory agencies.
This system emerged from the Tenth Amendment’s reservation of powers to states, establishing a regulatory framework where:
- Each state independently determines qualification standards for medical practitioners
- State medical boards serve as primary regulatory authorities
- Requirements for education, examination, and practice standards vary significantly across jurisdictions
- Renewal processes, continuing education requirements, and disciplinary procedures follow state-specific guidelines
The traditional model requires providers to obtain separate licenses in each state where they practice, creating administrative burdens that can impede workforce mobility and patient access to care.
The Growing Need for Multi-State Practice
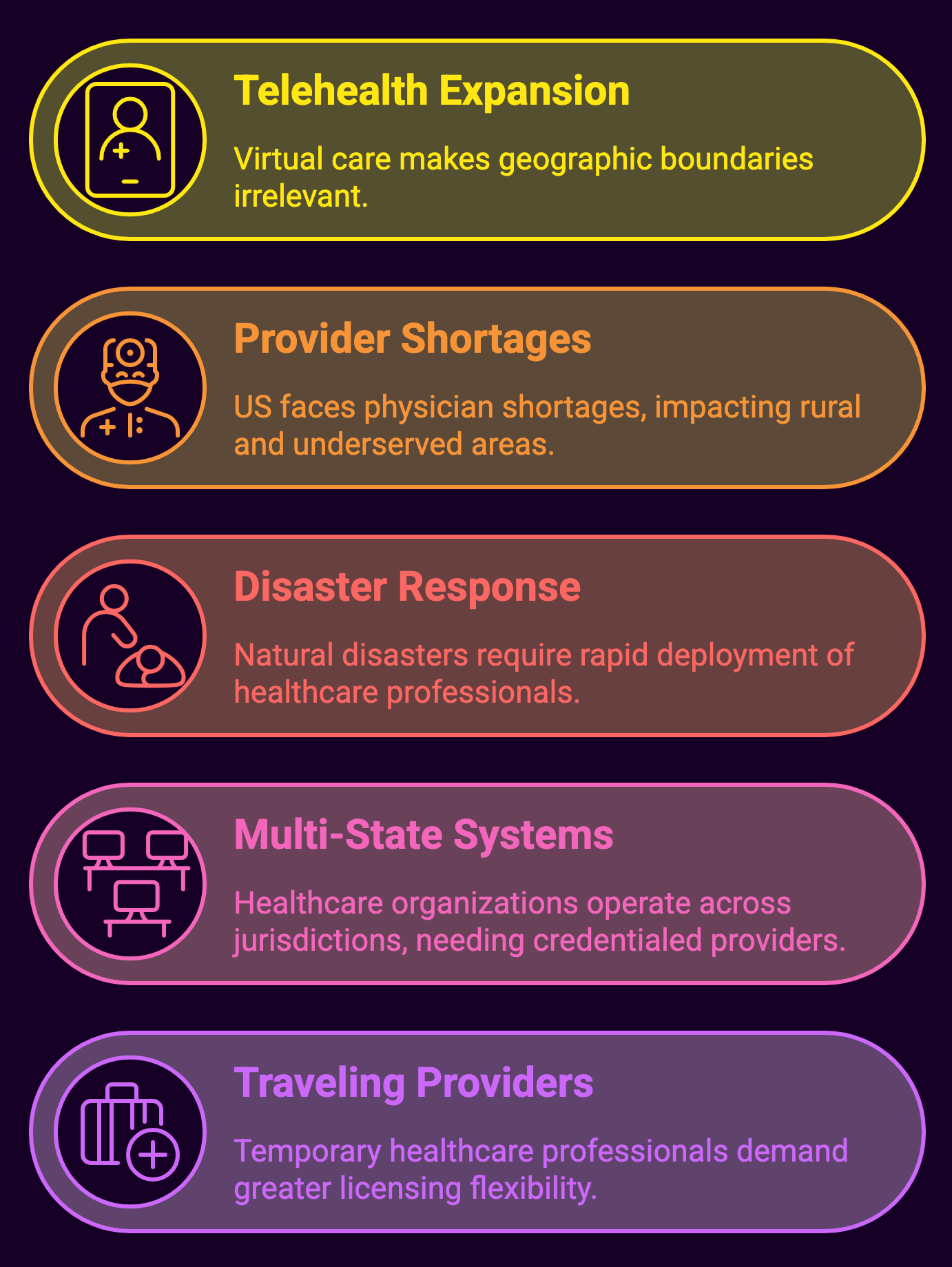
Several factors have accelerated the need for streamlined multi-state licensing:
- Telehealth Expansion: Virtual care delivery has rendered geographic boundaries increasingly irrelevant, especially following the COVID-19 pandemic when telehealth adoption increased by over 150% in many healthcare systems.
- Provider Shortages: According to the Association of American Medical Colleges (AAMC), the U.S. faces a projected shortage of between 37,800 and 124,000 physicians by 2034, with particular impacts in rural and underserved areas.
- Disaster Response: Natural disasters and public health emergencies require rapid deployment of healthcare professionals across state lines.
- Multi-State Health Systems: Large healthcare organizations increasingly operate across multiple jurisdictions, necessitating credentialed providers who can practice throughout their networks.
- Locum Tenens and Traveling Providers: The growing market for temporary and traveling healthcare professionals demands greater licensing flexibility.
Current Multi-State Licensing Models
Interstate Medical Licensure Compact (IMLC)
 The IMLC represents one of the most significant advances in multi-state physician licensing.
The IMLC represents one of the most significant advances in multi-state physician licensing.
Established in 2015, the compact:
- Creates an expedited pathway for qualified physicians to practice in multiple member states
- Maintains state-based regulatory authority while streamlining the application process
- Currently includes 40 states, the District of Columbia, and Guam as members
- Has processed over 25,000 applications since inception
- Reduces licensing timeframes from months to weeks for eligible physicians
To qualify for the IMLC pathway, physicians must:
- Hold a full, unrestricted medical license in a member state (designated as the state of principal license)
- Have completed an accredited medical education program
- Successfully completed USMLE or COMLEX-USA examinations
- Hold specialty certification or time-unlimited certification
- Have no history of disciplinary actions or criminal convictions
Nursing Licensure Compact (NLC)
The Nursing Licensure Compact, initiated in 2000 and enhanced as the eNLC in 2018, offers a model for registered nurses (RNs) and licensed practical/vocational nurses (LPNs/LVNs).
Key features include:
- Multistate license privilege allowing practice in all member states
- Current participation by 39 jurisdictions
- Uniform licensure requirements across participating states
- Enhanced public protection through coordinated disciplinary actions
- Recognition of both physical and remote nursing practice
The NLC has facilitated greater workforce mobility while maintaining public protection through coordinated information systems like Nursys, which tracks licensure and disciplinary actions across state lines.
Additional Profession-Specific Compacts
Other healthcare professions have developed similar interstate agreements:
- Physical Therapy Compact (PT Compact): Active in 33 states, allowing physical therapists to practice across member jurisdictions
- Psychology Interjurisdictional Compact (PSYPACT): Enabling telepsychology and temporary in-person practice across 36 member states
- Emergency Medical Services Compact (REPLICA): Facilitating cross-border practice for EMS personnel in emergency situations
- Audiology and Speech-Language Pathology Interstate Compact (ASLP-IC): Recently implemented with 23 member states
- Occupational Therapy Licensure Compact: Newest addition with growing membership
Credentialing Challenges in Multi-State Practice
Despite advances in interstate compacts, significant challenges persist in multi-state credentialing:
Administrative Burden and Costs
The financial and administrative impact of maintaining multiple state licenses remains substantial:
- Initial application fees ranging from $200-$1,000 per state
- Annual or biennial renewal costs of $100-$600 per state
- Varying continuing education requirements across jurisdictions
- Disparate background check processes and documentation needs
- Multiple malpractice insurance considerations
For healthcare organizations, these challenges extend to primary source verification, privileging processes, and ongoing monitoring of license status across multiple states.
Variability in Requirements
Significant inconsistencies exist across state regulatory frameworks:
- Education Verification: Some states require specific educational pathways or additional training
- Examination Standards: Different passing scores or examination requirements
- Background Check Processes: Varying fingerprinting and criminal history review methods
- Continuing Education: Differing hourly requirements and accepted course types
- Renewal Timelines: Asynchronous renewal cycles creating administrative complexity
Telehealth-Specific Considerations
Virtual care delivery introduces additional licensing complexities:
- Determining the “location of practice” (patient location vs. provider location)
- Varying telehealth-specific regulations and standards
- Cross-border prescribing limitations
- Reimbursement policies tied to licensing status
- Technology platform compliance requirements
Emerging Solutions and Best Practices
Centralized Credentialing Services
Healthcare organizations increasingly leverage centralized credentialing verification organizations (CVOs) and credentials verification services to streamline multi-state processes.
These entities:
- Maintain comprehensive provider data repositories
- Track licensing requirements across jurisdictions
- Automate renewal notifications and application processes
- Integrate with facility privileging systems
- Ensure compliance with accreditation standards (e.g., Joint Commission, NCQA)
Leading healthcare systems report 30-45% reductions in credentialing-related administrative costs through centralized approaches.
Technology Solutions
Digital innovation is transforming multi-state credentialing through:
- Blockchain-Based Credentials: Creating immutable, verifiable credential records that can be securely shared across jurisdictions
- Provider Data Management Platforms: Offering comprehensive, real-time tracking of licensing status
- Automated Primary Source Verification: Reducing manual verification processes through direct data exchange with licensing authorities
- Predictive Analytics: Identifying potential licensure issues before they impact practice eligibility
- API Integrations: Connecting credentialing systems with state medical boards, DEA databases, and other primary sources
Policy and Advocacy Initiatives
Several policy approaches aim to further streamline multi-state practice:
- Federal Preemption Proposals: Legislative initiatives to establish national licensing standards for certain provider types or practice settings
- Reciprocity Agreements: Bilateral arrangements between states recognizing each other’s licensing standards
- Telehealth-Specific Reforms: Policies addressing virtual care delivery across state lines, particularly for established patient relationships
- Standardization Efforts: Initiatives to harmonize application processes, verification standards, and continuing education requirements
- Delegation Models: Frameworks allowing healthcare organizations to assume greater responsibility for credential verification across multiple states
Implementation Strategies for Healthcare Organizations
Organizations supporting multi-state practitioners should consider these best practices:
Strategic Planning
- Assess geographic practice needs based on patient population and service delivery models
- Prioritize states based on provider mobility, telehealth requirements, and business objectives
- Consider compact membership status when developing multi-state strategies
- Establish policies for licensing reimbursement and support
Process Optimization
- Implement centralized tracking systems for license status, renewals, and requirements
- Develop standardized processes for initial applications across multiple jurisdictions
- Create clear workflows for maintaining multi-state credentials
- Establish monitoring mechanisms for regulatory changes affecting multi-state practice
Provider Support
- Offer dedicated resources for navigating multi-state licensing requirements
- Provide education on interstate practice regulations
- Consider financial support for multi-state licensing costs
- Develop clear policies on telehealth practice across jurisdictions
Future Directions and Trends
The landscape of multi-state licensing continues to evolve rapidly, with several notable trends emerging:
Expansion of Interstate Compacts
Existing compacts continue to add member states, while new profession-specific compacts are under development. The COVID-19 pandemic accelerated compact participation, with multiple states joining existing frameworks to address emergency workforce needs.
Telehealth-Driven Policy Evolution
Virtual care expansion is driving regulatory innovation, with several approaches gaining traction:
- Registration Models: Allowing out-of-state providers to register with state boards rather than obtaining full licensure
- Consultation Exceptions: Expanding traditional consultation exceptions to include ongoing telehealth relationships
- Patient-Centered Approaches: Regulations based on established relationships rather than geographic boundaries
National Standards Development
While maintaining state-based regulatory authority, efforts to develop consistent national standards are advancing through:
- Federation of State Medical Boards (FSMB) policy recommendations
- National Council of State Boards of Nursing (NCSBN) unified guidelines
- Accreditation standards promoting consistent credentialing processes
- Federal initiatives to reduce regulatory fragmentation
Data Sharing and Interoperability
Information exchange between credentialing systems, state boards, and healthcare organizations continues to improve through:
- Enhanced Provider Data Banks
- Standardized APIs for credential verification
- Real-time disciplinary action notifications
- Secure credential exchange protocols
Summary: A Multi-State Licensing Approach in Provider Credentialing
![]() Multi-state licensing represents one of the most significant challenges in modern healthcare credentialing, yet also offers tremendous opportunities to expand access to care, address workforce shortages, and support innovative delivery models. The continued evolution of interstate compacts, technological solutions, and policy frameworks provides a pathway toward a more streamlined system that maintains appropriate regulatory oversight while reducing unnecessary barriers to practice.
Multi-state licensing represents one of the most significant challenges in modern healthcare credentialing, yet also offers tremendous opportunities to expand access to care, address workforce shortages, and support innovative delivery models. The continued evolution of interstate compacts, technological solutions, and policy frameworks provides a pathway toward a more streamlined system that maintains appropriate regulatory oversight while reducing unnecessary barriers to practice.
Healthcare organizations, regulatory bodies, and individual providers must collaboratively navigate this complex landscape, advocating for evidence-based approaches that protect patients while enabling care delivery across traditional boundaries. With virtual care becoming increasingly central to healthcare delivery and provider shortages persist, the importance of efficient multi-state credentialing will only continue to grow, making strategic approaches to this challenge an essential component of healthcare workforce planning.

