Medical credentialing serves as a critical foundation for ensuring quality care and maintaining trust in our healthcare systems. This process, which verifies that healthcare providers meet established standards of education, training, and competence, involves numerous stakeholders who each play distinct yet interconnected roles. Finding out who these key players are and how they interact is essential for healthcare professionals, administrators, and even patients seeking to navigate this ecosystem effectively.
Healthcare Providers: The Starting Point
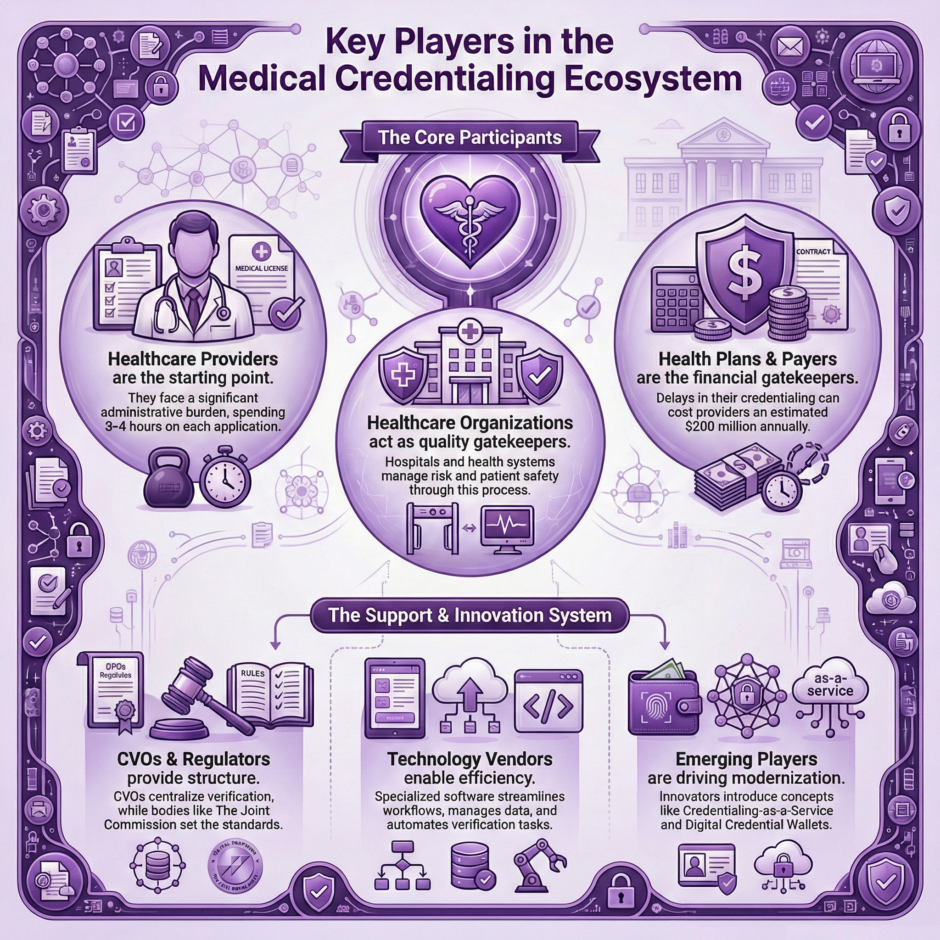
 At the core of the credentialing ecosystem are the healthcare providers themselves. Physicians, nurse practitioners, physician assistants, dentists, psychologists, and other clinical professionals. These individuals initiate the credentialing process as they seek to establish their professional legitimacy and gain the right to practice in various settings.
At the core of the credentialing ecosystem are the healthcare providers themselves. Physicians, nurse practitioners, physician assistants, dentists, psychologists, and other clinical professionals. These individuals initiate the credentialing process as they seek to establish their professional legitimacy and gain the right to practice in various settings.
For providers, credentialing represents both a professional milestone and an ongoing obligation. The process begins during their education and training and continues throughout their career. New graduates face particularly steep challenges as they assemble their credentials for the first time, gathering documentation of their degrees, residency completions, board certifications, and state licenses.
Established providers face their own challenges, as they must regularly renew credentials and maintain documentation of continuing education. Many providers practice across multiple facilities or insurance networks, resulting in numerous separate credentialing processes, each with its own timelines, requirements, and renewal cycles.
The administrative burden on providers can be substantial. According to industry surveys, physicians spend an average of 3-4 hours completing each credentialing application, with many completing multiple applications per year. This represents significant time away from patient care and contributes to physician burnout.
Healthcare Organizations: Gatekeepers of Quality
Hospitals, health systems, ambulatory surgery centers, and other care delivery organizations represent another critical segment in the credentialing ecosystem. These entities bear primary responsibility for ensuring that the providers who practice within their facilities meet established standards of competence and quality.
For these organizations, provider credentialing serves multiple purposes:
- Risk management and patient safety assurance
- Compliance with regulatory requirements
- Protection against potential liability claims
- Maintenance of institutional reputation and quality standards
Within these organizations, credentialing typically falls under the purview of the Medical Staff Services Department or similar unit. These departments employ Medical Staff Professionals (MSPs), specialists trained in the intricacies of provider verification and privileging processes. MSPs coordinate the collection and verification of provider credentials, facilitate review by appropriate committees, and maintain credential files.
The work of credentialing departments extends beyond initial verification to include:
- Ongoing monitoring of licenses, certifications, and sanctions
- Coordination of privileging processes that determine which specific procedures or services a provider can perform
- Regular reappointment reviews (typically every 2-3 years)
- Integration of performance data into credential files
For large health systems with dozens of facilities and thousands of providers, the credentialing function represents a significant operational investment, often supported by dedicated software systems and substantial staff resources.
Health Plans and Payers: Financial Gatekeepers
Insurance companies, managed care organizations, and government payers like Medicare and Medicaid constitute another key stakeholder group in the credentialing ecosystem. These entities credential providers before accepting them into their networks and authorizing payment for services.
For payers, credentialing serves as both a quality assurance mechanism and a means of controlling network composition.
The process allows them to:
- Verify provider qualifications before allowing them to bill for services
- Ensure compliance with state and federal regulations
- Maintain appropriate network adequacy and specialty distribution
- Implement value-based care initiatives by selecting high-performing providers
Payer credentialing typically includes verification of:
- Professional education and training
- Board certifications
- State licensure
- Malpractice insurance coverage
- Practice history and disciplinary actions
- Office accessibility and services
Health plans may also incorporate additional requirements related to their specific programs or standards. For instance, Medicare Advantage plans often include specific credentialing elements that align with CMS requirements, while plans focused on value-based care may incorporate quality metrics or cost-efficiency data into their credentialing processes.
The relationship between payers and providers around credentialing has historically been contentious. Providers frequently cite delays in payer credentialing, which can stretch from 90 to 180 days, as a significant barrier to practice and revenue generation. These delays contribute to the estimated $200 million in revenue lost by healthcare providers annually due to credentialing inefficiencies.
Credentialing Verification Organizations (CVOs): The Specialists
As credentialing complexity has increased, specialized entities known as Credentialing Verification Organizations or CVOs have emerged to streamline and standardize aspects of the process. CVOs serve as centralized verification services, collecting and validating provider information on behalf of hospitals, health systems, and health plans.
CVOs may operate as:
- Independent commercial businesses
- Services offered by state medical societies or hospital associations
- Departments within large health systems
- Regional collaboratives serving multiple healthcare organizations
The value proposition of CVOs centers on efficiency and standardization.
By centralizing verification tasks, they can:
- Reduce duplication of effort across organizations
- Standardize verification methodologies
- Achieve economies of scale in data collection
- Maintain relationships with primary sources
- Keep current with changing regulatory requirements
Some CVOs focus solely on primary source verification, the process of confirming credentials directly with issuing entities such as medical schools, residency programs, and licensing boards. Others provide more in-depth services, including application processing, committee support, and ongoing monitoring.
The rise of CVOs reflects the growing recognition that credentialing represents a non-competitive function that can benefit from industry collaboration. While hospitals and health plans may compete for patients and members, they share common interests in maintaining efficient, accurate credentialing processes.
Regulatory Bodies: Setting the Standards
State licensing boards, the Centers for Medicare and Medicaid Services (CMS), and accreditation organizations like The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) establish the regulatory framework within which credentialing occurs.
State medical, nursing, and other professional licensing boards serve as fundamental gatekeepers, determining who may legally practice specific professions within state boundaries.
These boards:
- Set minimum requirements for licensure
- Investigate complaints against providers
- Take disciplinary action when necessary
- Maintain publicly accessible databases of licensed professionals
CMS, as the administrator of Medicare and Medicaid programs, establishes conditions of participation that include specific credentialing requirements for healthcare facilities. These requirements cascade throughout the healthcare system, as CMS certification is essential for most hospitals and other provider organizations.
Accreditation bodies further codify credentialing standards and assess organizational compliance through regular surveys. The Joint Commission’s Medical Staff standards, for instance, provide detailed guidance on credentialing processes for hospitals and health systems. Similarly, NCQA’s Credentialing standards govern health plan credentialing activities and serve as the basis for their Health Plan Accreditation program.
These regulatory entities drive continuous evolution in credentialing practices.
Recent years have seen increased emphasis on:
- Ongoing professional practice evaluation rather than episodic reviews
- Integration of quality data into credentialing decisions
- Enhanced background screening requirements
- More rigorous verification of specific competencies
- Greater attention to provider wellness and burnout factors
Technology Vendors: Enabling Efficiency
The complexity of modern credentialing has driven the development of specialized software systems designed to streamline workflows, enhance compliance, and reduce administrative burdens. These technology vendors have become increasingly important players in the credentialing ecosystem.
Credentialing software systems typically provide capabilities for:
- Provider data management
- Document collection and storage
- Primary source verification tracking
- Expiration monitoring and alerts
- Committee review management
- Privileging process support
- Reporting and analytics
The market includes both established vendors with extensive credentialing solutions and newer entrants offering cloud-based platforms with innovative approaches. Many systems now incorporate artificial intelligence and machine learning to automate routine verification tasks and identify potential red flags in provider applications.
Beyond standalone credentialing systems, the ecosystem now includes technology platforms that facilitate data sharing across organizations.
For example:
- Provider data management systems that maintain current information for use across multiple credentialing processes
- Blockchain-based solutions that create verified, immutable records of provider credentials
- API-based integration services that connect disparate credentialing systems
These technologies are gradually addressing one of the most persistent challenges in credentialing: the redundancy of providers submitting the same information to multiple organizations. However, technical challenges around data standardization, system interoperability, and security concerns continue to hinder broader adoption of shared credentialing infrastructure.
Medical Societies and Provider Advocacy Groups: Representing Provider Interests
Professional associations like the American Medical Association (AMA), specialty societies, and state medical associations advocate for providers in credentialing matters and often develop resources to assist their members with navigating the process.
These organizations contribute to the credentialing ecosystem in several ways:
- Advocating for legislative and regulatory reforms to streamline credentialing
- Developing standardized forms and processes (such as the AMA’s Physician Profile service)
- Providing education and resources to help providers manage credentialing effectively
- Offering credentialing services directly or through affiliated organizations
- Participating in industry initiatives to improve credentialing efficiency
For example, many state medical societies operate their own CVOs or partner with commercial entities to offer credentialing services to their members. These society-sponsored CVOs often emphasize provider-friendly processes and advocate for their members when disputes arise with health plans or hospitals.
Professional associations have also been key drivers behind legislative efforts to establish standardized credentialing processes and timeframes at the state level. These “Any Willing Provider” or “Clean Credentialing Application” laws, which exist in various forms across numerous states, typically establish maximum processing times for credentialing applications and standardize information requirements.
Emerging Players: Innovators and Disruptors
The inefficiencies in traditional credentialing processes have attracted new entrants seeking to transform the ecosystem through innovative approaches and business models.
These emerging players include:
Credentialing-as-a-Service Providers
These companies offer end-to-end outsourcing of the credentialing function, handling everything from application completion to payer enrollment and ongoing maintenance. Unlike traditional CVOs that focus primarily on verification, these services aim to manage the entire credentialing lifecycle.
Digital Credential Wallets
Following models from other industries, these platforms allow providers to maintain verified digital versions of their credentials that can be securely shared with multiple organizations. The goal is to establish “verify once, use many times” capabilities that reduce redundant verification activities.
Provider Enrollment Networks
These collaborative platforms create shared infrastructure for health plans and providers to exchange credentialing information, often incorporating delegated credentialing arrangements that allow hospitals or large medical groups to credential providers on behalf of multiple payers.
Telehealth Credentialing Specialists
Specialized telehealth credentialing services have emerged to help virtual care providers navigate the complex maze of obtaining licenses and credentials across multiple states.
These innovators face significant challenges in gaining adoption within a highly regulated industry with established processes and powerful incumbents. However, they represent important voices pushing for modernization and efficiency in the credentialing landscape.
Patients: The Ultimate Stakeholders
While not directly involved in credentialing processes, patients represent the ultimate stakeholders in the credentialing ecosystem. Credentialing exists fundamentally to protect patients by ensuring that healthcare providers meet established standards of competence and quality.
Patients interact with the outputs of credentialing processes when they:
- Select providers from health plan directories (populated based on credentialing decisions)
- Receive care at hospitals or facilities that have granted privileges to their providers
- Access state licensing board websites to verify provider credentials or check disciplinary history
- File complaints that trigger investigations into provider qualifications or conduct
Increasing transparency has made some aspects of credentialing more visible to patients. Many state licensing boards now maintain public websites where patients can verify provider licenses and view disciplinary actions. Similarly, the National Practitioner Data Bank (NPDB), while not directly accessible to patients, influences credentialing decisions that ultimately affect patient care.
Patient advocacy organizations have also begun engaging more actively in credentialing policy discussions, particularly around issues of network adequacy, provider directory accuracy, and the inclusion of patient experience data in credentialing decisions.
The Path Forward: Integration and Collaboration
The medical credentialing ecosystem continues to develop in response to healthcare transformation, regulatory changes, and technological innovation.
Several trends point toward potential future directions:
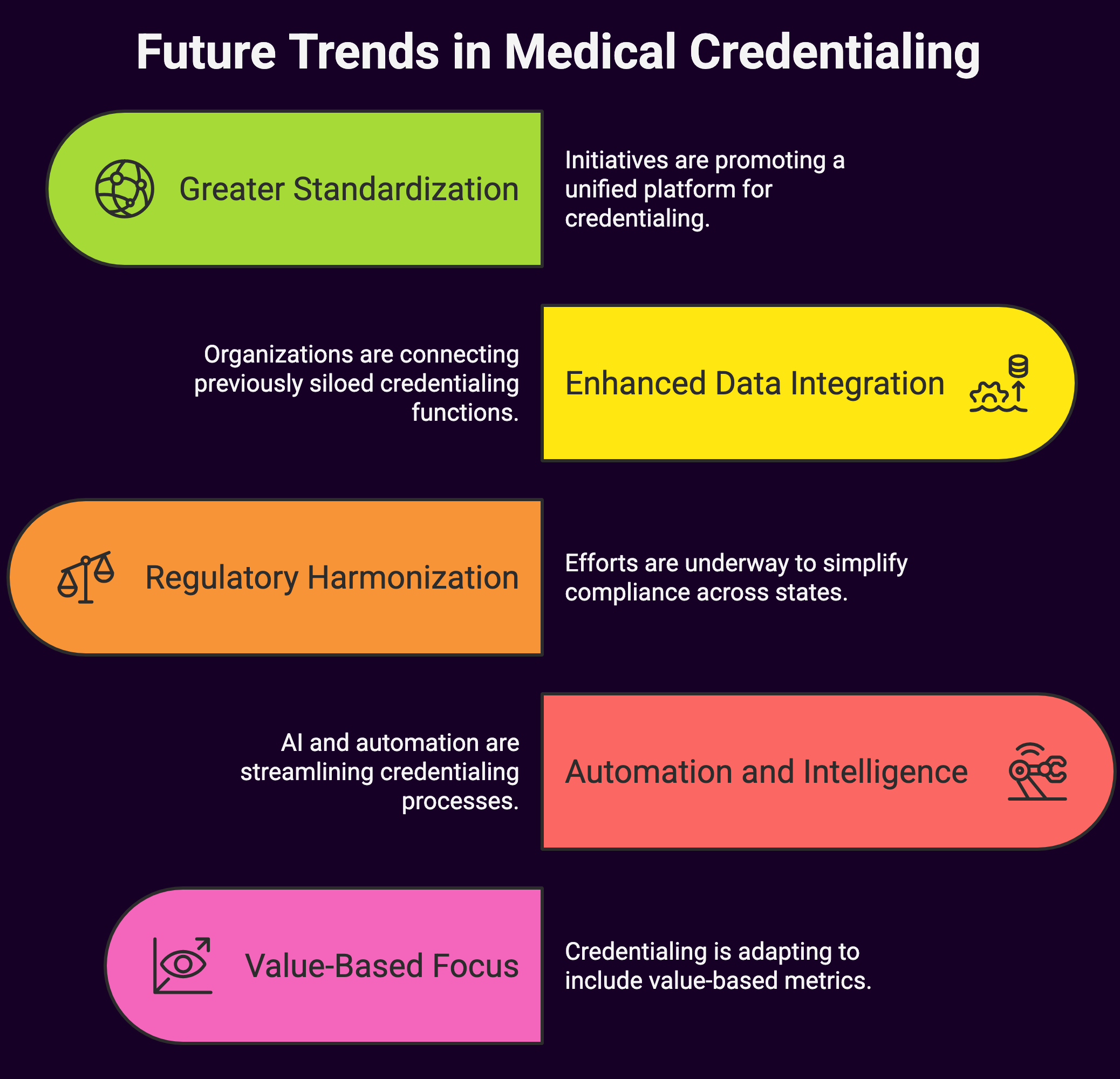
Greater Standardization
Industry initiatives like the CAQH ProView system, which provides a standardized platform for providers to submit and maintain their credentialing information, are gaining traction as stakeholders recognize the benefits of shared infrastructure.
Enhanced Data Integration
The walls between credentialing, privileging, performance improvement, and ongoing professional evaluation are gradually breaking down, with organizations increasingly seeking integrated approaches that connect these previously siloed functions.
Regulatory Harmonization
Efforts to reduce variation in requirements across states and accrediting bodies aim to simplify compliance and reduce administrative burden for both providers and healthcare organizations.
Automation and Intelligence
Artificial intelligence and robotic process automation are being applied to routine aspects of credentialing, reducing manual effort and accelerating processing times while potentially enhancing accuracy.
Value-Based Focus
Healthcare is shifting toward value-based payment models, hence credentialing processes are beginning to incorporate additional dimensions beyond traditional qualifications, including cost-efficiency metrics, patient experience scores, and outcomes data.
These developments suggest a future where credentialing processes become more efficient and less burdensome while simultaneously becoming more sophisticated in their ability to assess provider qualifications holistically.
Summary: Medical Credentialing Ecosystem Key Players
 The medical credentialing ecosystem encompasses a diverse array of stakeholders, each with distinct roles, responsibilities, and interests. Healthcare providers, delivery organizations, payers, specialized service providers, regulators, and technology vendors all participate in a complex web of interactions that ultimately serves to ensure provider competence and protect patient safety.
The medical credentialing ecosystem encompasses a diverse array of stakeholders, each with distinct roles, responsibilities, and interests. Healthcare providers, delivery organizations, payers, specialized service providers, regulators, and technology vendors all participate in a complex web of interactions that ultimately serves to ensure provider competence and protect patient safety.
An appreciation of these key players and their relationships provides valuable context for healthcare leaders seeking to navigate credentialing challenges or implement improvements in their own organizations. While the ecosystem remains fragmented and inefficient in many respects, ongoing efforts toward standardization, collaboration, and technological innovation offer promise for a more streamlined future state that better serves the needs of all stakeholders, especially the patients who rely on effective credentialing to ensure quality care.

