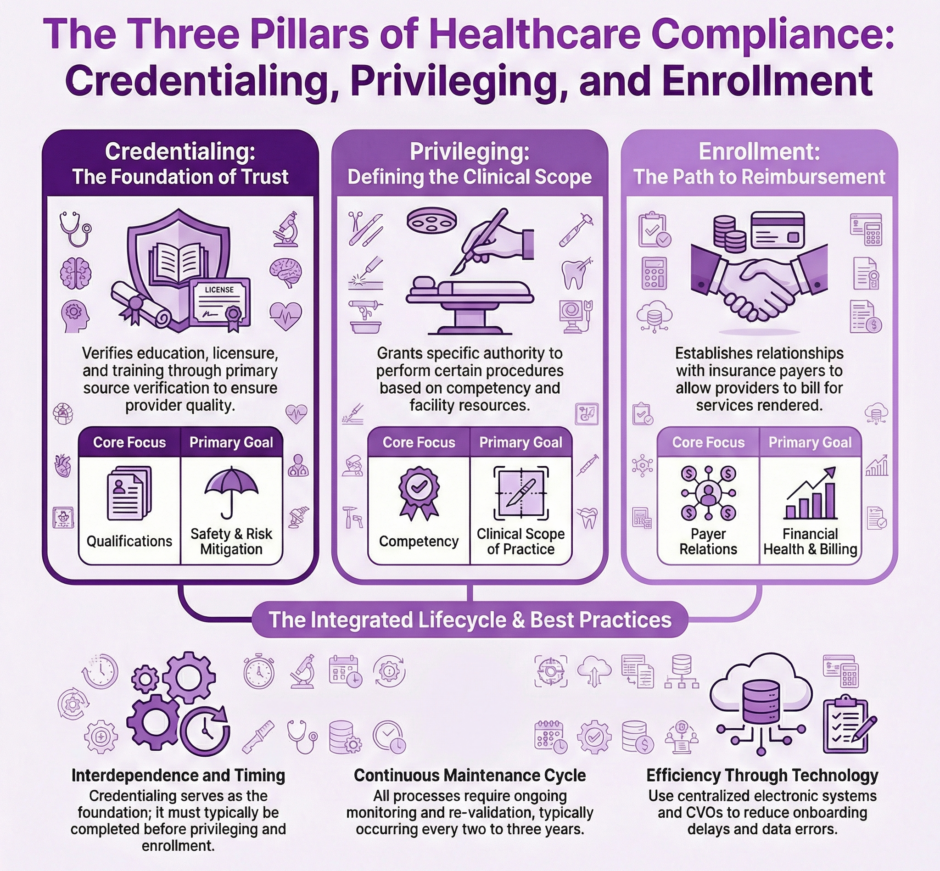
Three critical processes play a pivotal role in ensuring the quality, safety, and efficiency of patient care: credentialing, privileging, and enrollment. While these terms are often used interchangeably, they represent distinct yet interconnected procedures that healthcare organizations must navigate to maintain compliance, mitigate risks, and optimize their operations. Understanding the nuances of each process is essential for healthcare administrators, practitioners, and stakeholders alike.
Credentialing: Verifying Qualifications and Competence
Credentialing serves as the foundation for healthcare quality assurance. It is an in-depth process of collecting, verifying, and evaluating a healthcare provider’s qualifications, including their education, training, licensure, certifications, and relevant experience. The primary purpose of credentialing is to confirm that a practitioner possesses the necessary qualifications to provide safe and effective patient care within a specific healthcare setting.
Key Components of Credentialing:
 Primary Source Verification: This involves directly contacting the original sources of a provider’s credentials, such as medical schools, residency programs, and licensing boards, to confirm the authenticity of the information provided.
Primary Source Verification: This involves directly contacting the original sources of a provider’s credentials, such as medical schools, residency programs, and licensing boards, to confirm the authenticity of the information provided.- Background Checks: Credentialing often includes criminal background checks, verification of malpractice history, and checks against federal exclusion lists to ensure the provider has no disqualifying factors.
- Ongoing Monitoring: Credentialing is not a one-time event but a continuous process. Healthcare organizations must regularly re-credential providers, typically every two to three years, to ensure their qualifications remain current and valid.
- Compliance with Regulatory Standards: The credentialing process must adhere to standards set by accrediting bodies such as The Joint Commission, the National Committee for Quality Assurance (NCQA), and the Utilization Review Accreditation Commission (URAC).
- Documentation and Record-Keeping: Maintaining detailed records of the credentialing process is crucial for compliance, audit purposes, and potential legal challenges.
Credentialing serves as a critical risk management tool for healthcare organizations. Thoroughly vetting providers’ qualifications enables institutions to protect patients from unqualified practitioners and shield themselves from potential liability associated with negligent credentialing claims.
Privileging: Granting Specific Clinical Authorities
While credentialing establishes a provider’s qualifications, privileging determines the specific clinical activities a practitioner is allowed to perform within a healthcare facility. Privileging is a more focused process that considers not only a provider’s credentials but also their specific competencies, experience, and the needs of the healthcare organization.
Key Aspects of Privileging:
- Scope of Practice Definition: Privileging involves defining the exact procedures, treatments, or services a provider is authorized to perform. This can range from broad categories (e.g., “general surgery”) to highly specific procedures (e.g., “laparoscopic cholecystectomy”).
- Competency Assessment: Beyond credentials, privileging considers a provider’s demonstrated competence in specific areas. This may involve reviewing case logs, peer recommendations, and outcomes data.
- Facility-Specific Considerations: Privileging takes into account the resources, equipment, and support staff available at a particular healthcare facility. A provider may be qualified to perform certain procedures but may not be granted privileges if the facility lacks the necessary infrastructure.
- Tiered or Provisional Privileges: Some organizations use tiered privileging systems, granting provisional or supervised privileges to new practitioners before awarding full privileges.
- Regular Review and Renewal: Like credentialing, privileging is an ongoing process. Privileges are typically reviewed and renewed on a regular basis, often in conjunction with the re-credentialing cycle.
- Emergency and Disaster Privileges: Healthcare organizations must have processes in place for granting temporary privileges during emergencies or disasters when the normal privileging process may not be feasible.
Privileging is crucial for patient safety and quality of care. It ensures that providers only perform procedures and services for which they are competent and the facility is equipped to support. Effective privileging processes help minimize the risk of adverse events and improve overall patient outcomes.
Enrollment: Establishing Provider-Payer Relationships
Provider enrollment, often referred to as payer enrollment or insurance credentialing, is the process by which healthcare providers establish relationships with insurance companies, government programs (like Medicare and Medicaid), and other payers. This process allows providers to bill for services rendered to patients covered by these payers and receive reimbursement.
Key Elements of Enrollment:
- Payer-Specific Requirements: Each payer may have unique enrollment criteria and processes. Providers often need to enroll separately with multiple payers.
- Documentation Submission: Enrollment typically requires submitting extensive documentation, including proof of licensure, malpractice insurance, board certifications, and often information already collected during the credentialing process.
- Provider Networks: Enrollment often involves joining a payer’s provider network, which may have additional requirements or contract negotiations.
- Credentials Verification Organizations (CVOs): Many payers use CVOs to streamline the enrollment process, reducing redundancy in information gathering and verification.
- Ongoing Maintenance: Like credentialing and privileging, enrollment requires regular updates and renewals to maintain active status with payers.
- Compliance with Payer Policies: Enrolled providers must adhere to the payer’s policies, billing practices, and quality metrics to maintain their enrollment status.
- Revalidation: Government programs like Medicare require periodic revalidation of enrollment information to ensure continued compliance with program requirements.
Provider enrollment is critical for the financial health of healthcare organizations and individual practitioners. Proper enrollment ensures timely and accurate reimbursement for services, reduces claim denials, and allows providers to serve a wider patient population.
Interrelationships and Distinctions
While credentialing, privileging, and enrollment are distinct processes, they are closely interrelated and often interdependent:
- Credentialing as a Foundation: Both privileging and enrollment typically rely on the information gathered and verified during the credentialing process. A robust credentialing system can streamline privileging and enrollment procedures.
- Scope and Focus: Credentialing is the broadest process, focusing on overall qualifications. Privileging narrows the focus to specific clinical competencies within a particular facility. Enrollment is primarily concerned with establishing the business relationship between providers and payers.
- Timing and Sequence: Credentialing usually precedes privileging, as privileges cannot be granted without first verifying qualifications. Enrollment may occur concurrently with or after credentialing and privileging, depending on the provider’s and organization’s circumstances.
- Regulatory Oversight: While all three processes are subject to regulatory oversight, the specific governing bodies and standards may differ. Credentialing and privileging are heavily influenced by healthcare accreditation organizations, while enrollment is largely governed by payer-specific rules and government regulations.
- Lifecycle and Renewal: All three processes require ongoing management and periodic renewal, but the timelines and requirements for each may vary.
Challenges and Best Practices
Healthcare organizations face several challenges in managing credentialing, privileging, and enrollment processes:
- Data Management: Collecting, verifying, and maintaining large volumes of provider data can be time-consuming and error-prone. Implementing robust healthcare information systems and leveraging technology solutions can help streamline these processes.
- Regulatory Compliance: Keeping up with changing regulations and standards across multiple accrediting bodies and payers is challenging. Organizations should invest in ongoing education and training for staff involved in these processes.
- Timeframes and Efficiency: Lengthy credentialing, privileging, and enrollment processes can delay provider onboarding and impact revenue. Implementing centralized verification organizations (CVOs) and adopting standardized forms like the Council for Affordable Quality Healthcare (CAQH) ProView can improve efficiency.
- Balancing Thoroughness and Expediency: Organizations must strike a balance between conducting thorough vetting processes and avoiding unnecessary delays in provider onboarding.
- Coordination Across Departments: Effective management of these processes requires coordination between various departments, including medical staff offices, human resources, legal, and finance. Clear communication channels and well-defined workflows are essential.
Best practices for managing these processes include:
- Implementing centralized, electronic systems for managing provider data and documentation.
- Establishing clear policies and procedures for each process, including defined timelines and responsibilities.
- Regularly auditing and evaluating the effectiveness of credentialing, privileging, and enrollment processes.
- Providing ongoing education and training for both administrative staff and healthcare providers on the importance and requirements of these processes.
- Leveraging industry standards and shared databases to reduce redundancy in data collection and verification.
- Implementing continuous monitoring systems to alert organizations to changes in provider status (e.g., license expiration, disciplinary actions) between formal re-credentialing cycles.
Summary: Credentialing, Privileging, and Enrollment Differentiation
![]() Credentialing, privileging, and enrollment are distinct yet interconnected processes crucial to the functioning of healthcare organizations. Credentialing ensures that providers have the necessary qualifications and background to practice safely. Privileging defines the specific clinical activities a provider can perform within a given healthcare setting. *We’ve written about credentialing versus privileging. Enrollment establishes the business relationships necessary for providers to be reimbursed for their services.
Credentialing, privileging, and enrollment are distinct yet interconnected processes crucial to the functioning of healthcare organizations. Credentialing ensures that providers have the necessary qualifications and background to practice safely. Privileging defines the specific clinical activities a provider can perform within a given healthcare setting. *We’ve written about credentialing versus privileging. Enrollment establishes the business relationships necessary for providers to be reimbursed for their services.
Knowing the nuances of each process and their interrelationships is essential for healthcare administrators, providers, and payers. Implementing robust systems and best practices for managing these processes allows healthcare organizations to enhance patient safety, improve operational efficiency, and ensure regulatory compliance.
With increasing emphasis on quality metrics, value-based care, and technological integration, the importance of effective credentialing, privileging, and enrollment processes will only grow. Healthcare organizations that excel in these areas will be better positioned to deliver high-quality care, maintain financial stability, and navigate the complex regulatory environment of modern healthcare.
Contact us to handle all of your credentialing, privileging, and enrollment needs and / or challenges.


 Primary Source Verification: This involves directly contacting the original sources of a provider’s credentials, such as medical schools, residency programs, and licensing boards, to confirm the authenticity of the information provided.
Primary Source Verification: This involves directly contacting the original sources of a provider’s credentials, such as medical schools, residency programs, and licensing boards, to confirm the authenticity of the information provided.