Let’s be real – medical billing can be a huge pain. For those who perform it internally and externally. At times, it’s one of those mind-numbingly tedious tasks that makes you question your career choices. Hours upon hours of copying and pasting data from one system to another, checking and re-checking codes, filling out endless forms. It’s enough to make you want to run screaming into the night.
But what if I told you there’s a better way? A way to automate all that drudgery and let computers do the heavy lifting? That’s where robotic process automation (RPA) comes in. It’s revolutionizing medical billing by taking those monotonous manual entry tasks off your plate.
Now you’re probably thinking “Great, just what I need – another buzzword and newfangled techno-thing to wrap my head around.” But stick with me here, because once you see how RPA works its magic, you’ll be an absolute convert.
The Essence of RPA
At its core, RPA is software that mimics human actions within computer applications. It’s like having a hyper-efficient digital employee working 24/7, automatically transferring data, triggering actions, and following rule-based processes. Anywhere there’s a repetitive, routine task to be done, RPA can swoop in and knock it out.
In medical billing, RPA tackles some of the most tedious and error-prone duties like:
- Collecting patient info across different systems
- Verifying insurance coverage and eligibility
- Entering procedural and diagnosis codes
- Submitting claims to payers
- Posting payments
- Dealing with claim rejections and appeals
Basically, all those monotonous jobs that have you zoning out and making silly mistakes – those are prime targets for automation with RPA.
The RPA Difference
Now you might be thinking “Can’t we already do some of that with traditional software?” And you’d be right…to an extent. Things like electronic health records (EHRs), billing software, and practice management systems have brought some automation to medical billing.
But here’s the key difference – those old-school solutions are very rigidly designed and integrated. They only “talk” to each other in fairly limited ways. RPA, on the other hand, operates at the user interface (UI) level. It can seamlessly jump between different applications, websites, databases…you name it. It’s way more flexible and versatile.
Another massive advantage? You don’t need to rip-and-replace your existing tech stack. RPA layers right on top, making those legacy systems way smarter and more automated. It’s like duct-taping a turbocharger onto your old beater. Except, you know, more advanced than duct tape.
The consistency factor is also huge. Humans are bound to make mistakes when stuck doing boring, repetitive work all day. We space out, miss things, accidentally fat-finger entries. Robotic software doesn’t have those “oopsie” moments. It follows processes with robotic precision every single time. That translates to fewer errors, rejections, and denial write-offs in medical billing.
Show Me the Money
I can hear the bean counters among you asking “Yeah, but what’s the bottom line here? How much can RPA actually save my practice?” Buckle up, because the ROI numbers are pretty staggering.
Research from Intelligent Automation Universe pegs the overall cost savings from using RPA in healthcare revenue cycle management at around 65%. That’s no small potatoes. Let’s put some concrete numbers to those percentages:
Say your medical billing team consists of 10 full-time employees pulling $40K salaries on average. That’s $400K per year just in wages. If RPA can take over and automate 65% of their workload, you’re looking at $260K in annual savings. Sure, the software itself costs money to implement. But industry stats show RPA typically pays for itself within 6-9 months.
And we’re just looking at direct payroll costs. RPA driving down denial rates and speeding up payments cranks the revenue spigot even higher. In fact, the automation firm Prosolutions found that by automating their medical billing processes, their healthcare clients boosted revenue 40% year-over-year while reducing costs 60%. Those are some seriously fat stats.
The Skeptics’ Take
I know what you’re thinking: “This all sounds great in theory, but what about the real-world practicalities? Surely there are some downsides to this whole RPA business?”
Fair enough, let’s address some common skepticisms:
- “My medical billing is too complex and unique for robots.”
Yeah, every healthcare provider likes to think their situation is a precious little snowflake. But RPA tools today are crazy advanced and customizable. With some upfront configuration, they can absolutely handle even the most convoluted processes and workflows. - “What about security and compliance? I can’t just hand over all my sensitive data.”
Valid concern, but most quality RPA platforms are built with robust security controls, audit trails, encryption, and privacy safeguards baked right in. And processes can be designed to follow all the same protocols as humans. - “Alright, but what about the technical skills required? I don’t have a bunch of developers on staff.”
This might’ve been an issue in RPA’s early days, but now the tools are much more user-friendly. With visual drag-and-drop builders and pre-built process templates, even non-techies can design and implement automations without writing code. - “But robots are going to take all our jobs! What happens to my billing team?”
Realistically, full robotic replacements of entire roles are still a longways off. RPA’s strengths are in automating highly specific, repetitive tasks that humans find soul-crushing anyway. Your skilled billing pros can be reassigned to higher-value work requiring judgment, customer service, and creative thinking.
The Automated Future
At this point, you’re probably ready to run out and implement all the RPA all over the place, right? Whoa, let’s pump the brakes a second. As transformative as this automation can be, it’s not something to rush headlong into without a plan.
The dirty little secret? Most RPA initiatives never reach their full potential or fizzle out due to poor implementation and change management. You’ve got to start with a thorough process mining phase to identify the right candidates for automation and map out your approach.
Don’t just assume decades-old billing processes are still optimized – RPA is a great opportunity to eliminate unnecessary steps or bypass clunky legacy apps entirely. You’ll also want to phase things in strategically across departments, monitor and tweak automations, retrain staff… it’s a whole change journey.
But when healthcare organizations do take the measured, strategic approach?
The results can be downright game-changing for medical billing:
- Stanford Hospital saw a 92% reduction in their billing department’s workload from RPA
- A top orthopaedic practice doubled their billing efficiency and increased reimbursement speed 80%
- HCA Healthcare’s robotic billing process averages over 600,000 automated transactions per month
Numbers like that make it really, really tough to keep doing things the old, manual way. As RPA keeps maturing and becoming more accessible, every advantage argues for getting on board sooner rather than later.
I know what you’re thinking now: “Enough with the theoretical soapboxing already. Just show me how this RPA stuff works!” Ask and you shall receive…
A Peek Under the RPA Hood
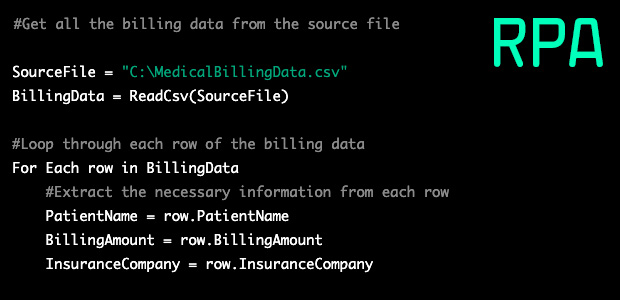
Let’s walk through a simplified example of how automated medical billing via RPA might work at your practice.
We’ll start with a bot extracting charges from your EMR system each night for the following day’s patient visits:
- RPA logs into the EMR and navigates to the report-running screen, entering the required date and facility filters
- It extracts the report data to a CSV file and saves it to a network share
- Now the bot jumps over to your practice management system and logs in
- Following a set of rules, it parses through the CSV data, mapping EMR charges to the correct patient accounts and populating charges, codes, modifiers, etc.
- Typically, any incomplete data is flagged for human review before final charge entry
Seem pretty straightforward so far? Now let’s add another layer of automation:
- As charges are posted, the bot runs a cross-check against each patient’s insurance eligibility and benefits
- If an Auth or pre-certification is required, it automatically sends compliance requests to the payer with all needed documentation
- Once cleared, the charge gets scheduled for claim submission in the billing queue
Boom, just like that, your claims are prepped with way fewer manual touchpoints and double-handling! But the robotic automation isn’t done:
- Each morning, the EMR data extraction is cross-referenced against new co-pay, deductible, or policy updates received overnight via EDI feeds
- Warnings or rejected charges get routed to billing staff work queues before claim finalization
- Approved primary claims are then automatically submitted to clearinghouses
Can you see how this entire billing lifecycle is getting streamlined through the interconnected RPA workflows? The bot keeps all the data unified and applies billing rules without errors as it marches from system to system.
Heck, that’s barely scratching the surface. With the right extended process automations, you could have your robot:
- Monitoring claim statuses and triggering automated follow-ups
- Auto-posting payments and adjustments per contracted rates
- Handling claim rejections, appeals, resubmissions
- Generating self-service payment reminder comms with patient portals
And data flows both ways – the robot feeds info back into upstream EHR and PM systems for things like denial management, claim editing, and medical coding optimization according to your business rules.
This is just one illustrative example, but hopefully you can begin to see how RPA represents a comprehensive upgrade to medical billing processes from top to bottom. No more fragmented data, re-keying, or manual cross-checks between patients, insurers, providers, and facilities. The automation gains are exponential.
How to Start RPA’ing Your Rev Cycle
So you’re sold on the transformative potential of RPA for your medical billing operations, but now you’re wondering – how do I even get this show on the road?
Here’s a quick-hit to-do list to becoming an RPAing pro:
- Choose a platform with strong healthcare-specific capabilities and support. Don’t try launching an enterprise automation rollout all footloose and fancy-free. The right RPA vendor is critical.
- Identify your initial automation candidates through process mining. Look for repetitive, rules-based billing processes with high volumes of consistent data flows across multiple systems. These will yield your quickest wins.
- Map out your processes visually from end-to-end. You need to meticulously detail every step, application, data source, decision rule, etc. Nothing can be assumed for the bot’s logic.
- Build comprehensive test environments for developing and refining your bots. You don’t want software screwing up data integrity in your live production systems!
- Train your billing staff as bot builders and orchestrators. Let them own the robotic processes to maximize buy-in, while IT handles governance and upkeep.
- Consider low/no code solutions to simplify buildout. Drag-and-drop automation canvases can let non-techies get up and running faster.
- Start small with an RPA pilot before scaling practice- or enterprise-wide. Iterative rollouts let you solidify procedures and address snags early on.
- Don’t just automate crappy procedures for crappy procedures’ sake. See RPA adoption as an opportunity to streamline and refine suboptimal workflows.
- Make sure you have centralized governance models for reusability. Once bots are built, share processes and data flows throughout the organization as templates.
- Build a culture of continuous improvement. Just because you’ve automated something doesn’t mean you’re done. Always be refining!
No one’s saying RPA deployment is a cakewalk. It requires planning, resourcing, employee training and buy-in…you’ve got to be all in. But when you stack the long-term efficiencies and savings against the upfront lift, it’s one of the biggest no-brainer investments your revenue cycle operations can make.
The Future is Automated (For Real This Time)
We’ve been hearing about the “automated future” of healthcare for ages now, but RPA finally represents a shortcut to realizing that long-promised utopia. Unlike previous generations of workflow automation technology, RPA’s lowered barrier to entry is making it increasingly feasible for practices of any size to start harnessing its power.
At the end of the day, this isn’t about cutting costs and head counts (though those are welcome side effects). It’s about allocating your most precious resources more intelligently – having skilled humans focus on the strategic, analytical, and relational aspects of medical billing while robotic workhorses churn through the tedious grunt work in perfect lockstep.
Pretty soon, the idea of manually keying claims or rekeying data between systems for hours on end will seem as antiquated as paper records or dictation machines. As the leaders in RPA adoption are already proving, it won’t just be a competitive edge… but a baseline necessity for survival.
So look, you can either slowly suffocate under the escalating administrative bloat of healthcare reimbursement. Or you can uncork the pent-up potential of automation, and let your billers and coders escape the drudgery for higher-value pursuits. RPA is here. It’s robust, proven, and profoundly effective at ramping medical billing into the 21st century.
The only remaining question is: will your organization embrace the future, or be subsumed by it?